Before diving into the antibiotic cascade, let’s review some basic terms pertaining to antibiotic reporting and other principles.
Definition of Terms
MIC – Minimal Inhibitory Concentration is the minimal amount of antibiotic needed to inhibit bacterial growth. Provides a quantitative result using 3 or more dilutions of a particular antibiotic and is usually measured in milligrams per microliter.
AST – Antimicrobial Susceptible Testing is the actual testing of specific bacteria against different antimicrobial agents.
E-Test – Commercial test strip impregnated with varying concentrations of an antibiotic; used to determine the MIC of a particular microorganism.
KB – Alternative method of measuring an organism’s sensitivity or resistance to a particular antibiotic. Determined by using a disk impregnated with an antibiotic and measuring the zone of clearing (zone of inhibition) surrounding the disk. This method provides a qualitative result.
Breakpoint – a chosen concentration of antibiotic that defines when a particular bacteria is susceptible, resistant, or intermediate to that antibiotic.
How Antibiotic Reporting Normally Works
The purpose of antibiotic reporting is to give the clinicians the information they need to properly treat their patients. Pathogenic organisms are tested to determine which antibiotics they are sensitive or resistant to and thereby which antibiotics would be most useful to treat the patient’s infection. The type of antibiotics tested and subsequently reported to the patient’s record is based on a few things.
- Component of bacteria’s cell wall (is it gram-positive or gram-negative?).
- Organism group (Enterobacterales, Staphylococcus, Pseudomonas, Enterococcus, etc.).
- Specimen source (wound, respiratory, CSF, genital, etc.).
- Recommendations from infectious disease experts and pharmacy.
Based on the above criteria most labs will selectively report antibiotics. This means that antibiotics will only be released into the patient’s report if they are deemed appropriate for that site, type of bacteria, and recommendations. These criteria can be programmed into the laboratory information system or AST instrument.
What is the Antibiotic Reporting Cascade?
So what makes cascade reporting unique? Why is different from selective reporting or selective testing? Let’s find out.
Antibiotic Cascade Reporting Defined
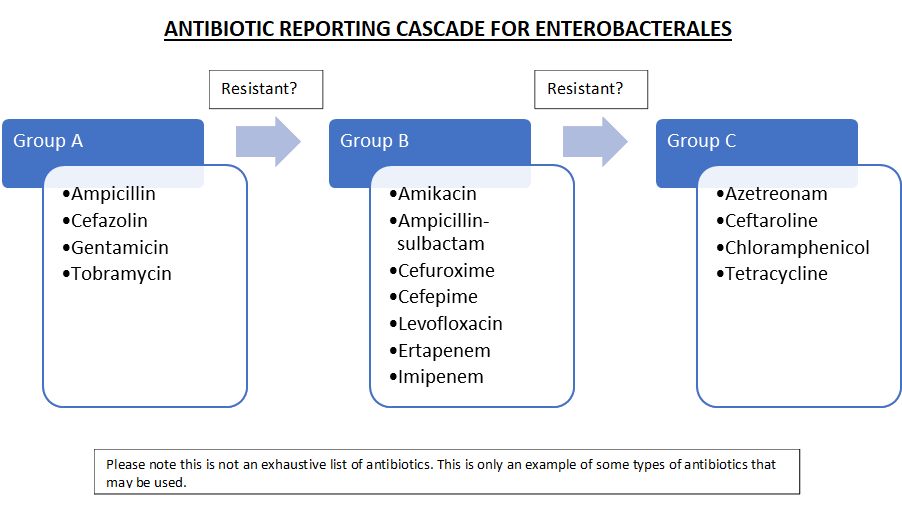
Antibiotic cascade reporting is a way of reporting antibiotic sensitivities in which secondary antibiotics are only reported if primary antibiotics for a particular organism exhibit resistance. See the example below for Enterobacterales. All recommended antibiotics are tested using traditional commercial AST devices, however, antibiotics in each subsequent group are only released if there is a resistant antibiotic in the previous group.
Difference Between Cascade Reporting, Selective Reporting, and Selective Testing
Many medical laboratory scientists who are familiar with antimicrobial susceptibility testing know that, in many cases, not all antibiotics are reported all the time. This is an example of selective reporting. Selective reporting limits what antibiotics are reported on specimens based on specific sources, patient age, or the type of bacteria. Examples include:
- Not reporting certain antibiotics such as doripenem, ertapenem, and imipenem on CSFs because they don’t cross the blood-brain barrier.
- Not reporting daptomycin on specimens from the respiratory tract.
- Reporting Tedizolid on E. faecalis isolates only.
Like cascade reporting, all antibiotics are tested but only some are released to the patient report.
Selective testing is similar to selective reporting. In this case, only appropriate antibiotics are tested for the specific site. Looking at the above example an organism isolated from a CSF wouldn’t even be tested for doripenem, ertapenem, or imipenem. This method is less wasteful, however, it creates problems when a physician wants a drug that is not normally used because they would have to wait an extra 24 hours to get results.
Why is the Antibiotic Reporting Cascade Important?
Utilizing the antibiotic cascade seems like a lot of extra work. Why put it to use? What are the benefits?
How Does it Help Patients?
Cascade reporting helps patients in many different ways. The primary way it helps is that cascade reporting cuts down on the time patients spend on antibiotics. This in turn helps to ensure that the organism the patient is infected with does not develop resistance to broad-spectrum antibiotics. The patient’s infection is more easily maintained and less likely to reoccur.
How Does it Help Clinicians?
Cascade reporting helps point the clinicians toward the right course of treatment. Most physicians are not experts when it comes to what kind of antibiotics are the most appropriate for treatment. Utilizing the cascade enables the physician to quickly change the patient’s treatment to a more appropriate course of antibiotic therapy.
How Does it Help the Hospital?
There are a few ways that antibiotic cascade reporting can help the hospital. The first way is that it helps the hospital save money. By ensuring that the correct and most effective antibiotics are used patients are cured faster and discharged earlier. Cascade reporting also helps to improve hospital-wide statistics on hospital-acquired infections.
How to Implement Antibiotic Cascade into Your Laboratory
It has been established what the antibiotic cascade is and how it can be helpful to clinicians, the hospital, and patients. How should it be implemented? It seems very confusing.
Updating procedures and validation
Before implementing any new test procedures must be updated. The procedure should include the antibiotic formularies, detailed descriptions of the antibiotic cascades, how antibiotics should be released, and MIC breakpoints for all antibiotics. Medical laboratory scientists then need to be trained on these new procedures.
Building Rules into LIS and Instrument
Implementing a new procedure like antibiotic cascade reporting can be hard and confusing. Programing rules into the LIS, middleware, or instrumentation can help. Programming rules into the computer software would allow the technologist to easily release the next group of antibiotics needed based on reporting rules.
Involving Infection Control, Infectious Disease, and Pharmacy
Involving infection control, infectious disease and pharmacy are of the utmost importance. These are the departments that are most directly involved in patient care. Their input will be valuable when creating the formulary. While most antibiotic cascade reporting closely follows CLSI guidelines, the cascade can be modified to best fit the organization’s needs.
Administrative Buy-in
Lastly, implementing an antibiotic cascade affects the entire organization. When implementing a policy that is this wide-reaching it is important to have the upper administration’s support. In order to obtain this, it is important to show how this will not only help the patients but how it will help the organization by saving money. Studies have shown that after implementing antibiotic cascade FTEs do go up, however, cost savings in other areas offset this. The antibiotic cascade can help cut costs in types of antibiotics used, length of hospital stays, length of treatment, and infection reoccurrence.

