A superbug is a microscopic organism (bacteria, virus, or fungus) that causes infection and is unable to be treated with commonly used drugs. These superbugs are often very difficult to treat and have a tendency to spread to other areas of the body, sometimes causing sepsis. They can also spread to other people. (NOTE: Some parasites can also be superbugs, but will not be discussed here.)
How do microorganisms become superbugs?
Microorganisms (let’s collectively call them germs from this point forward) are hearty little buggers. They adapt and do whatever they can to survive. In the world of germs, this adaptation is known as mutation.
Some germs mutate simply through natural evolution. Others adapt to the environment in which they reside.
Doctors prescribe antimicrobial medications (let’s simply refer to these as drugs) to treat infections based on patient symptoms and the area of the body that is affected (skin, urine, etc.). When a drug is prescribed, the hope is that it will kill the infective germ. Sometimes the drug prescribed doesn’t work and the doctor prescribes a different medication.
When treated with a drug, germs try to adapt to the new drug environment. If successful, mutations occur in their DNA, which allows them to survive and become unaffected by the prescribed drug. This is known as drug resistance. These germs continue to multiply and a different drug must be prescribed.
An example of mutation and drug resistance
Penicillin was released in 1941 and was used to treat a number of bacterial infections. One type of infection commonly treated with penicillin was Staphylococcus aureus (Staph aureus). However, some strains of Staph aureus started to become resistant to penicillin in 1942. Doctors then started treating these infections with methicillin.
Methicillin became the drug of choice for Staph aureus infections. Then in 1960, methicillin-resistant Staph aureus (commonly known as MRSA – pronounced “mersa”) reared its ugly head. This meant that MRSA was treated with the antibiotic of last resort – Vancomycin via IV, which can be nephrotoxic (cause kidney damage).
It’s a vicious cycle
MRSA can be very dangerous and can easily spread to others, especially in a hospital environment (but also in everyday life). But it hasn’t stopped there. In 2002, Vancomycin-intermediate and -resistant strains of Staph aureus (VISA and VRSA) began to appear and pharmaceutical companies developed new drugs to combat these superbugs.
A novel drug is a drug that has not previously been approved by the Food and Drug Administration (FDA) and European Medicines Agency (EMA). Novel drugs were created to deal with VISA and VRSA. Some of these were:
- Daptomycin (Cubicin®, Cubist Pharmaceuticals, Lexington, MA, USA)
- Linezolid (Zyvox®, ZyvoxID®, Pfizer, NY, USA)
- Tigecycline (Tygacil®, Wyeth Pharmaceuticals, NJ, USA)
- Quinupristin/dalfopristin (Synercid®, Monarch Pharmaceuticals, Bristol, TN, USA)
- Ceftobiprole (Zeftera, Basilea, Basel, Switzerland, in cooperation with Johnson & Johnson, Raritan, NJ, USA)
Newer strains of Staph aureus have adapted and are now able to resist treatment from some of these drugs.
How do germs mutate?
Germs develop defense strategies known as resistance mechanisms. They do this in several ways. They:
- Avoid using the drug’s target by developing new cell processes.
- Use enzymes to change or destroy the drug.
- Change the entryways or limit the number of entryways to restrict access by the drug.
- Change the drug’s target so that it can no longer fit and do its job.
- Use internal pumps to get rid of the drug.
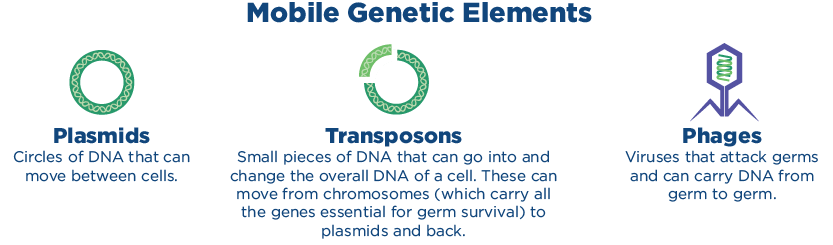
Resistance traits in germs can be inherited from generation to generation. They can also pass directly from one germ to another through mobile genetic elements. These elements include:
- Plasmids – Circles of DNA that can move between cells
- Transposons – Small pieces of DNA that can go into and change the overall DNA of a cell. These can move from chromosomes to plasmids and back.
- Phages – Viruses that attack germs and carry DNA from one germ to another.
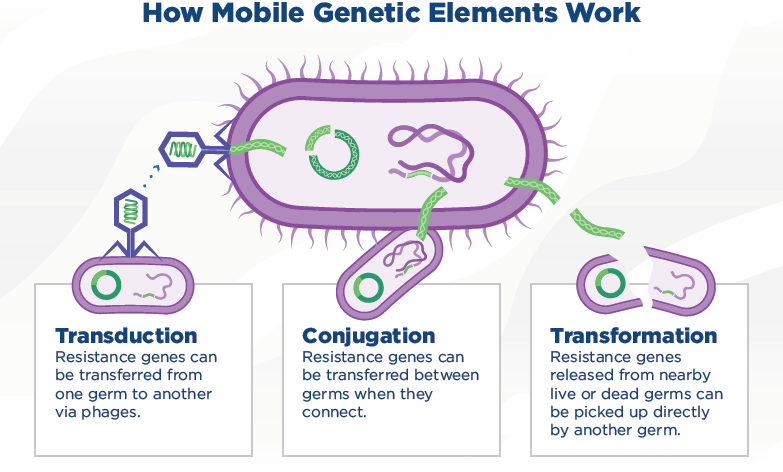
How do mobile genetic elements pass between microorganisms?
Mobile genetic elements pass between germs through one of three different processes. These processes are:
- Conjugation – Germs that touch or connect transfer resistance genes between them.
- Transformation – Nearby live or dead germs can directly pick up resistance genes from another germ.
- Transduction – Phages (viruses that infect other germs) can transfer resistance genes from one germ to another.
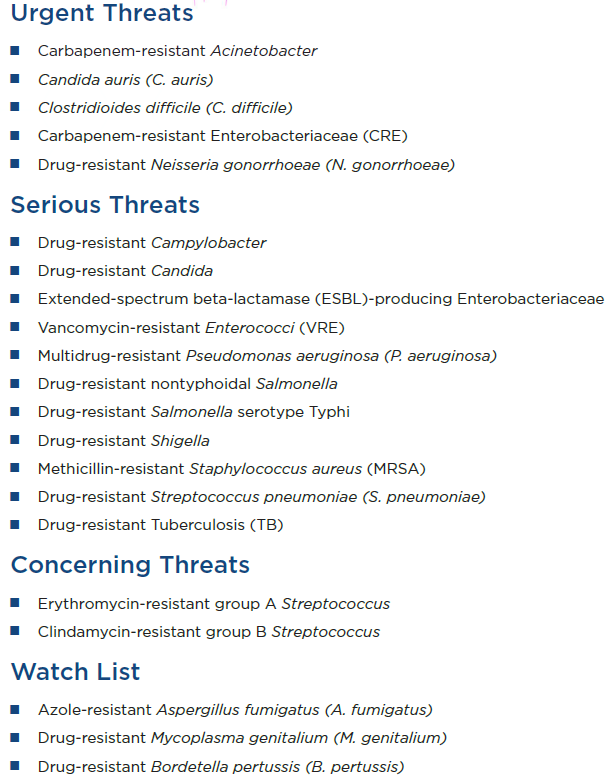
What are the biggest superbugs we face at this time?
The Centers for Disease Control and Prevention (CDC) periodically publishes a report that lists antibiotic threats in the United States. The latest report contains data from 2019. The full 2019 Antibiotic Resistance Threat Report, including methods and appendices, is available here.
Below are some of the most current threats.
How can we prevent more superbugs from developing?
- Wash your hands! Handwashing should take place frequently and each washing should be done with soap for at least 20 seconds. A common tip given to help you know how long to wash is to sing through the Happy Birthday song twice. When completed, you have adequately washed your hands.
- Take drugs for the entire prescribed timeframe, even if you feel better. Remember, germs can mutate by adapting to their environment. If you take a drug and it hasn’t completely destroyed the germ, mutations can occur.
- Do not take unnecessary antibiotics for colds, etc. Antibiotics treat bacterial infections and some fungal infections and are ineffective for viruses. When you have leftover antibiotics (which you shouldn’t) and begin taking them for a viral infection, they will disrupt normal “good” bacteria in your body and may make other bacteria resistant. Clostridioides difficile, commonly called C. diff, is a normal intestinal bacteria and does not cause problems when “good” intestinal bacteria are in balance. When good bacteria become unbalanced, C. diff takes over and causes a dangerous condition. This is primarily caused by frequent or unnecessary antibiotic use.
- Physicians and other clinicians should prescribe drugs cautiously and sparingly to prevent germs from mutating to become superbugs. When possible, wait for culture results before treatment.

