In the highly regulated world of healthcare, it seems as if the laboratory and hospital are in a constant state of inspection preparedness. At any given time, The Joint Commission, CAP, CMS, or local department of health can come waltzing in to turn your life upside down. Losing accreditation by one of these organizations can affect reimbursements or worse yet shut the hospital down. To avoid either of these scenarios painstaking care is often taken to ensure regulatory compliance, but what happens when you forget to check your CLSI antimicrobial standards?
What is CLSI?
CLSI stands for Clinical Laboratory Standards Institute. It is a not for profit membership organization dedicated to fostering excellence in laboratory medicine. The CLSI creates laboratory standards based on input from and consensus among industry, government, and health care professionals.
This is great but why do we need it?
Answer: Standardization
Standardization improves quality and efficiency of testing which ultimately contributes to better patient care.
Important Definitions
Minimum Inhibitory Concentration (MIC) – the lowest concentration of an antibiotic that prevents visible growth of a microorganism.
Breakpoint – chosen concentration of an antibiotic that defines whether a microorganism is susceptible or resistant to an antibiotic.
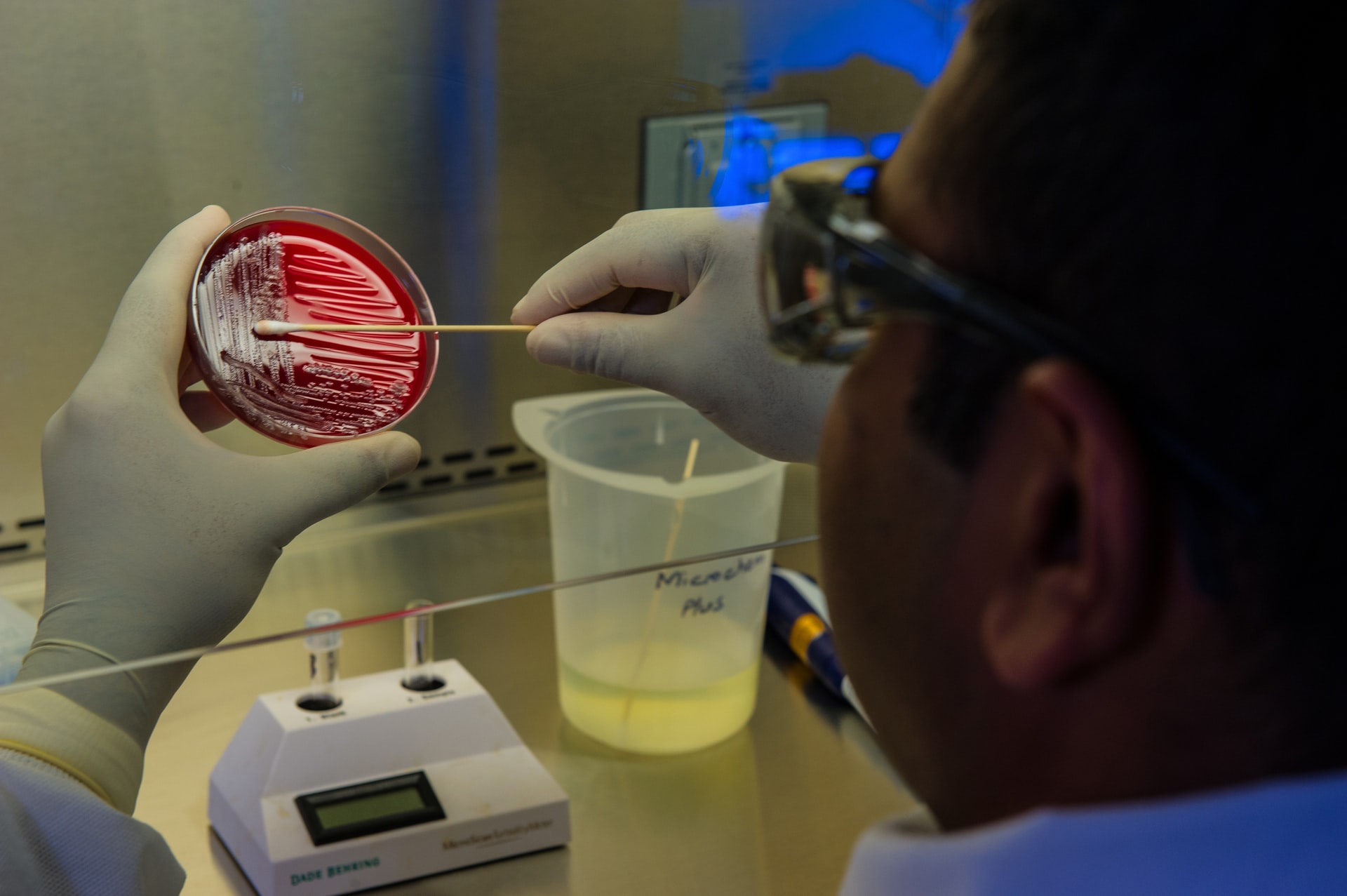
Kirby-Bauer – antibiotic sensitivity test in which disks impregnated with antibiotic media are implanted onto an agar plate that contains a lawn of bacteria. Plates are incubated for 24 hours. At the end of incubation, the zone size around each disk is measured and the size is used to determine sensitivity.
Take a look at this scenario:
A patient goes into the ED with a urinary tract infection. A urine sample is collected and a culture and sensitivity is ordered. The patient is sent home with antibiotics and told to follow up with their PCP. At the follow up appointment the PCP collects another urine sample from the patient and sends the specimen to a reference lab for another culture and sensitivity. When the physician receives the results a few days later she notices the MIC of the antibiotic the patient was given in the ED has increased.
Let’s imagine in the above scenario laboratories were allowed to set their own ranges for antibiotic MICs. If this were the case, then the elevated MIC would mean absolutely nothing to the doctor. This is why it is imperative that there is the same set of standards for every laboratory to follow.
What are the Processes for Establishing Breakpoints and Quality Control Ranges?
The CLSI develops its standards by a consensus method using an open forum within the health care industry. Anyone who has an interest in diagnostic patient care is able to participate. The CLSI Subcommittee on Antimicrobial Susceptibility Testing reviews data from a variety of sources in order to establish test methods, MIC breakpoints, and QC parameters.
The CLSI and its Contribution to Antibiotic Stewardship
The CLSI has a set of standards for every area of the laboratory. One of the most well known of these sets is probably the M100 Performance Standards for Antimicrobial Susceptibility Testing. This set of standards lists out everything you would ever want to know about each different class of bacteria, which antibiotics to use and their MIC breakpoints. The M100 is a truly comprehensive source for all things antibiotics and is reviewed and updated on a yearly basis.
Useful Sections of the M100
The M100 gives extremely detailed information on every aspect on antibiotic testing. To go over every single section of the M100 would be too much. Instead 3 sections will be the focus.
Tables 1A, 1B, and 1C: Officially these tables consist of “Suggested Groupings of Antimicrobial Agents Approved by the US Food and Drug Administration for Clinical Use That Should Be Considered for Testing and Reporting on Nonfastidious Organisms by Microbiology Laboratories in the United States.” These are suggested antibiotics to use for certain classes of bacteria and specimen sources.
These tables group antibiotics into 4 groups. Group A are the first choice drugs. Group B are the second choice drugs to be used in situations when antibiotics in group A are unavailable or cannot be used. Group C are supplemental antibiotics and group U are antibiotics to be used for UTIs only.
Tables 2A-2J: These tables are divided up by different classes of bacteria. For each class MIC breakpoints and Kirby-Bauer (KB) zone sizes are listed for all appropriate antibiotics. Special instructions are also given for when it is okay to use KB zone sizes or MIC only.
Tables 5A-5G: These tables focus specifically on QC organisms. MIC breakpoints are listed for each QC organism. Table 5G focuses on MIC trouble shooting.
It is important to note that for each of these tables there are foot notes and addendums for certain antibiotics and MIC ranges. It is very important that these not be disregarded. Often times these notes include important information regarding when it’s appropriate to use antibiotics. For example, for Salmonella and Shigella only a limited number of drugs should be reported. It is also important to carefully read through all the information in these sections as special exceptions for certain drugs may not be listed specifically in the table.
Don’t Ignore Your Antibiotics!
Because the M100 is updated every year the microbiology lab should also take care to review their antibiotic MIC breakpoints and rules. This is extremely important. Why? Because bacteria mutate and develop resistance. Year to year the MIC breakpoints and rules might not change that much, but what happens to a particular breakpoint in 5 years? If the lab doesn’t stay on top of antibiotic stewardship they could inadvertently begin to report out wrong sensitivities.
Consider the scenario in the previous section. The bacteria itself could have developed resistance, but it’s highly unlikely resistance would have developed in such a short time span. A more likely cause of this discrepancy is that the hospital laboratory was using an old set of antibiotic ranges and the reference laboratory had more up to date ranges.
Updating Your Lab’s Antibiotics
Ranges and Breakpoints: Updating these are easy. All that needs to be done is simply cross-check the ranges and breakpoints in the M100 standards with the ranges and breakpoints on your instrument.
Rules: This is a little more complicated. Rules for certain antibiotics can change depending on the specimen source and class of bacteria. Extensive cross-checking must occur in order to ensure the right antibiotics are being reported for each type of bacteria and each source. At this point, it would be a good idea to engage the technical representative for your instrument to help you review and write new rules. Language is very important. If a mistake is made with one word the consequences could be disastrous. (Maybe this is an overstatement but you will certainly have a lot of annoyed doctors.)
QC: This is also a fairly simple task. When checking ranges, breakpoints and rules for patient results take the time to do the same for QC. Bacterial QC strains mutate and change just like wild bacteria. QC ranges and breakpoints, as well as recommended QC for each biochemical test, should be checked on a yearly basis.
Barriers to Keeping up with MIC Breakpoints
If keeping MIC breakpoints and antibiotic rules is so important why do a lot of laboratories leave antimicrobial stewardship as an after thought?
- Time: This should be self-explanatory. Most labs are short-staffed and there are a million projects going on. Tasks in which the completion does not affect the immediate functioning of the lab get knocked down on the priority list.
- Solution: Designate a set time that a yearly review of MIC breakpoints should be completed and signed off by the medical director.
- Knowledge: This is more apparent in smaller community hospitals in which there may not be a full microbiology lab. Large medical centers have staff, including lab techs, supervisors, and a medical director, that specialize in that particular area. In a smaller lab, the techs are often generalists, knowing a little bit about each area but not really an expert in any one thing.
- Solution:
- Engage your instrument’s technical support.
- If affiliated with a larger medical center consult with pathologists at that site.
- Use a consulting firm.
- Access to Information: CLSI updated standards have to be purchased. This presents a struggle for already cash strapped health care organizations. The M100 costs $54.00 for members and $153.00 for non-members.
- Solution: The CLSI has recognized that cost is a problem for many labs and has made their M100 standards available for free online.
- Confusion: The M100 isn’t the easiest of books to read. The information is presented in such a way where the reader is required to flip back and forth between pages and refer to completely different sections of the book. There are many notes and addendums that the tech must pay attention to it can be easy to lose track.
- Solution:
- Be very careful when reading.
- Consult other labs in the area and compare notes.
In Summary…
CLSI breakpoints and antibiotic rules should not be ignored. It is the laboratory’s job to ensure that they are reporting out proper sensitivities to physicians. Antibiotic sensitivities should be resulted and comparable to other organizations.
To ensure that the results are standardized, the laboratory should review its antibiotic rules and MICs on a yearly basis. The M100 Performance Standards for Antimicrobial Susceptibility Testing is now offered for free online to help ensure that every laboratory has access to the most current and up to date standards available.

Great blog! This is very helpful for someone like me who has not done micro since I was in school in 1993. 🙂
Thank you!!