Approximately 70% of medical decisions are based on clinical laboratory results on all types of patient specimens (blood, urine, tissue, etc.).
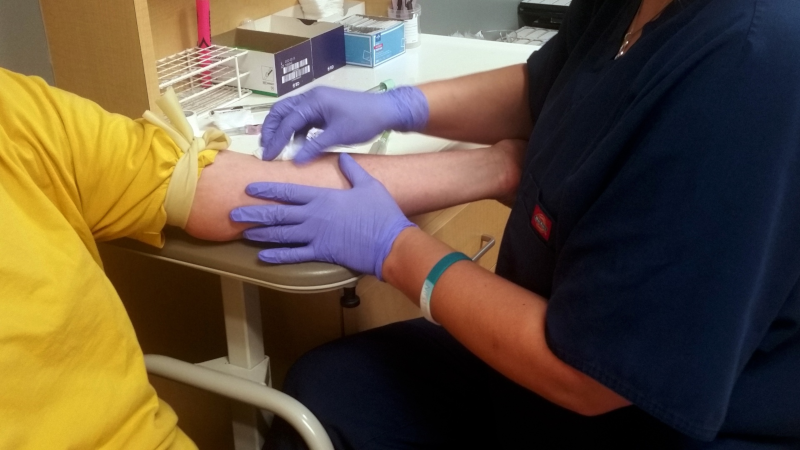
Phlebotomists collect blood samples from patients and process all types of laboratory specimens so they can be tested in the clinical laboratory. Good soft skills are paramount for phlebotomists, as they deal with patients from all age groups for a procedure that many deem as unpleasant. A patient’s encounter with the phlebotomist is what gives them their overall perception of the entire laboratory.
Simply put, phlebotomists are the front line and the face of the clinical laboratory and should be praised and respected as such.
Where do phlebotomists work?
There are many different settings where phlebotomists are employed. The majority likely work as part of the clinical laboratory in a hospital or medical center. However, there are other places of employment for phlebotomists. Listed below are a few examples.
– Other hospital departments such as cancer treatment, same-day surgery
– Physician group practices
– Blood donation centers
– Privately-owned clinical laboratories
– Insurance companies that require precertification
– Traveling phlebotomists hired for in-home or nursing home collections
Having both procedural skills and theoretical, conceptual knowledge is what makes a good phlebotomist and prevents many pre-analytical laboratory errors.
What education and training is required to work as a phlebotomist?
Technically, the only education required to work as a phlebotomist is a high school diploma (or equivalent). Phlebotomy procedures and skills can be taught through on-the-job training. However, I say this with caution, as more and more healthcare facilities are requiring phlebotomists to be nationally certified, and with good reason (to be discussed later).
The actual step-by-step procedure of collecting a blood sample from a patient is something that can be taught through on-the-job training (the procedural skills, or the ‘how’). However, it is not enough to only know how to perform procedural phlebotomy skills. It is also important to be able to understand and explain why things are done in a particular manner, as well as what can happen if someone deviates from the procedure (the theoretical, conceptual knowledge, or the ‘why’). Having both procedural skills and theoretical, conceptual knowledge is what makes a good phlebotomist and prevents many pre-analytical laboratory errors.
Training a new phlebotomist on the job is very time consuming and requires adequate staffing and close supervision. Unfortunately, much on-the-job training only focuses on procedural phlebotomy skills. This typically happens due to a lack of time due to increased workload and a lack of adequate training staff.
What are pre-analytical laboratory errors?
Clinical laboratory testing is broken down into three phases: pre-analytical, analytical, and post-analytical.
The pre-analytical testing phase includes anything that is done before actual clinical testing is performed on a patient sample. This phase includes things related to:
– patient identification
– patient preparation and preparation of collection site
– specimen collection (time, container, order of draw, etc.)
– specimen labeling
– specimen handling/transport/storage
– unacceptable specimens (hemolysis, contamination, etc.)
All of these items are performed by phlebotomists and unfortunately, this pre-analytical phase of testing is where most laboratory errors occur. However, it’s often not phlebotomists that are to blame.
Not everyone that collects blood samples is a phlebotomist.
If you are taken to a hospital via ambulance, an Emergency Medical Technician (EMT) or Paramedic will usually collect blood samples when they start an intravenous (IV). Blood samples in the emergency room are now typically collected by a nurse (RN or LPN) when an IV is started, or by an emergency room technician. Urgent care facilities and physician groups often hire medical assistants because they also take vitals in addition to collecting blood samples. Nurses collect blood samples on dialysis patients while they are having dialysis (at the end of the procedure). Nurses (RNs, sometimes a special IV team) collect blood samples from patients that have indwelling catheters such as a mediport. And finally, a physician may collect a blood sample when absolutely necessary (often from the femoral artery).
Testing on all blood samples must be performed in an accredited clinical laboratory, whether collected by a phlebotomist or any of the other professionals listed above. Trust me, in a very busy environment, phlebotomists are very grateful that other professionals are able to collect blood samples and get them to the clinical laboratory. However, most pre-analytical laboratory errors occur on specimens that are collected outside of the clinical laboratory staff. In other words, properly trained and educated phlebotomists are usually not to blame.
Why are many healthcare institutions requiring nationally certified phlebotomists?
As previously mentioned, many healthcare facilities are now requiring phlebotomy certification, both for current phlebotomists and new hires. Some of these facilities do not require every phlebotomist to be certified, but those that do have certification are typically rewarded with more pay or more enticing benefits.
In order to pass a national certification exam, a phlebotomist should have a background in the theory of:
– anatomy & physiology of the circulatory system,
– specimen collection for venipuncture and skin puncture,
– specimen processing and handling, and
– laboratory operations (HIPAA, safety, infection control, etc.).
Having a national phlebotomy certification reassures a clinical laboratory or HR department that specific standards and criteria have been met by an applicant or current employee. It affirms that an individual has both the procedural skills and theoretical, conceptual knowledge required to perform the essential tasks needed for their phlebotomy profession.
The certification organization that is the gold standard in national certification for many different clinical laboratory professions and specialties is the American Society for Clinical Pathology (ASCP). For phlebotomy certification, clinical training and orientation must be done in an accredited clinical laboratory.
ASCP has seven different routes that would qualify an individual to be eligible to take the Phlebotomy Technician certification exam. To see the eligibility requirements specific for the ASCP Phlebotomy Technician certification exam:
1. First, click here.
2. Click on U.S. Certifications.
3. Under Technician Certifications, click on PBT.
4. Click each of the seven different Eligibility Routes to see details.
To see a breakdown of exam content areas for the ASCP Phlebotomy Technician exam, download the content guidelines below. (Information obtained from the ASCP Board of Certification website.)
To see eligibility requirements for other less stringent phlebotomy certification associations, you can check out these links.
American Medical Technologists (AMT)
National Healthcareer Association (NHA)
Wrapping it up
From a bottom-line perspective, hiring certified phlebotomists saves time and money, and improves overall patient outcomes. On-the-job training time can easily be cut in half or better. Think of it this way…
More certified phlebotomists = Fewer pre-analytical errors.
Fewer pre-analytical errors = Fewer venipunctures for the patient.
Fewer venipunctures for the patient = Faster turn-around-time (TAT) for lab results.
Faster TAT for lab results = Faster patient treatment.
Faster patient treatment = Better patient outcomes.
Better patient outcomes = Better patient satisfaction and increased confidence/appreciation for the clinical laboratory (by both patients and physicians).
My personal opinion is that EVERYONE that collects patient blood samples should be trained and educated by a certified phlebotomist (PBT), a certified medical laboratory technician (MLT), or a certified medical laboratory scientist (MT or MLS).
It is important to have both the procedural skill of obtaining a blood sample AND the theoretical, conceptual knowledge of phlebotomy. Understanding why things are done a certain way and how deviating from a procedure can cause poor patient outcomes is critical.
Phlebotomists are the face/front line of the laboratory.
Praise them and respect them as such!

Great article!
Unfortunately, phlebotomists are often not given the respect they deserve. It takes more than just sticking a needle into a vein to get a quality blood sample. No matter how good a job we do after the sample is collected, it is all for naught if we don’t start with a quality sample.
Thank you for your advocacy!
Thanks so much, Chris!