Have you ever had an “a-ha moment” when an event happens and your memory is immediately triggered to something you were taught many years prior? That’s what happened to me while working an evening shift as a medical technologist at a small, rural hospital.
Our evening shift phlebotomist was busy, so I was called to the Emergency Department (ED) to collect blood on a young girl that was probably age 6 or 7. The girl was very thin, crying, and had mannerisms of a child much younger than her age. While there, I also retrieved a urine specimen that had already been collected on the same patient and then quickly returned to the lab to begin analyzing the patient’s specimens.
Working as one of only two techs on the evening shift, I became very adept at multi-tasking. I put the blood tube for chemistry testing in the centrifuge, placed the blood tube for hematology on the tube rocker to thoroughly mix, and proceeded to urinalysis to perform the first part of the urine testing. The instant I removed the lid from the urine specimen I was hit with the overwhelming smell of maple syrup. AHA!
Should I mention anything about my observation?
After we completed all testing and released the results in the computer, I called the ED and asked to speak to the physician that was taking care of this patient. I explained that the patient’s urine sample had the overwhelming smell of maple syrup and told the doctor I recalled learning that this could be indicative of maple syrup urine disease.
The ED doctor thanked me for this information and shared that this child was basically a “failure to thrive” case. He said the information I provided was very helpful and actually fit perfectly with the patient’s symptoms of weakness, sluggishness, poor appetite, and abnormal muscle tone.
What is Maple Syrup Urine Disease (MSUD)?
Maple Syrup Urine Disease (MSUD) is a life-threatening metabolic disease that is diagnosed in early childhood. The disease gets its name from the sweet maple syrup or burnt sugar smell of the urine in untreated children. This sweet smell may also be noticed in the child’s sweat or earwax.
MSUD is a rare inherited disease affecting only 1 in every 185,000 births. It is an autosomal recessive disorder, where both mother and father are considered carriers and have no symptoms. It occurs more frequently in the Mennonite community (or other populations with a small gene pool), or when close relatives (i.e., cousins) have children together.
There are four (4) main types of MSUD. They are:
- Classic – This is the most severe form of the disease and usually develops within the first three (3) days of birth.
- Intermediate – This is less severe than classic MSUD and appears in children between 5 months of age and 7 years old.
- Intermittent – These children can usually tolerate higher levels of leucine, isoleucine, and valine. They typically develop as expected and only show symptoms after an infection or another type of stress.
- Thiamine-responsive – These children respond well to high doses of thiamine (vitamin B1) along with a restricted diet. When treated, they tend to have a higher tolerance for leucine, isoleucine, and valine.
What causes MSUD?
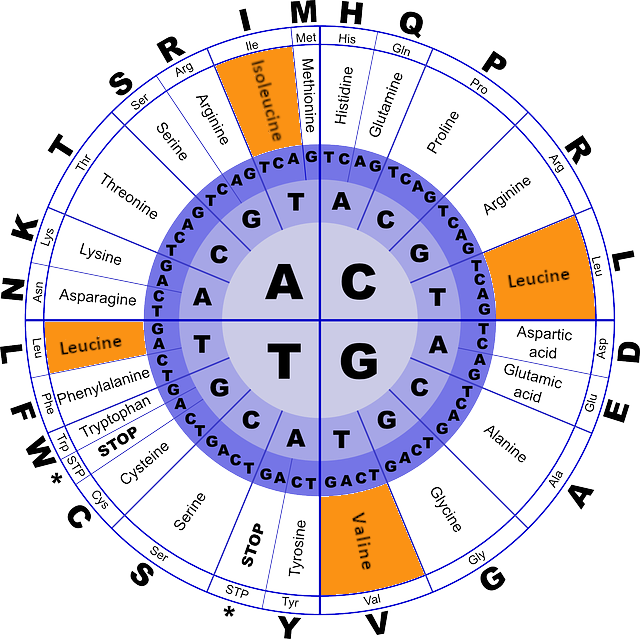
MSUD is caused by a mutation of one of three different genes: BCKDHA, BCKHB, and DBT. A mutation in any one of these produces a non-working gene and results in the absence or decreased activity of branched-chain ketoacid dehydrogenase (BCKAD) enzymes.
BCKAD enzymes are necessary to break down amino acids leucine, isoleucine, and valine that are present in all proteins. These three amino acids are known as branched-chain amino acids (BCAAs). Since MSUD patients are unable to break down these three BCAAs, high levels of BCAAs build up in the body, become toxic, and can cause severe health problems including brain damage or death.
Both parents of a child with MSUD are carriers, which means they each have one working copy of the gene and one non-working copy of the gene. Since MSUD is an autosomal recessive disease, a child with MSUD inherits a non-working gene copy from each parent.
Children born to parents that are carriers have a 25% chance of being affected by MSUD, a 50% chance of being a carrier with no symptoms, and a 25% chance for the child to be completely unaffected (no disease and a non-carrier).
What are the signs and symptoms of MSUD?
All four types of MSUD listed above have common symptoms.
- Urine, sweat, or earwax with the telltale smell of maple syrup or burnt sugar.
- Severe weakness (lethargy).
- Learning problems/Developmental delay/Poor growth.
- Poor feeding/Loss of appetite/Vomiting.
- Irritability.
- Poor muscle tone/Muscle spasticity (backward arching of the head, neck, and spine).
- Seizures/Convulsions/Respiratory failure/Coma may be seen as the condition progresses.
How is MSUD officially diagnosed?
- If a child has the characteristic maple syrup odor of their urine plus other symptoms of MSUD, that can be diagnostic enough to begin therapy followed by more diagnostic testing.
- All states in the U.S. offer newborn screening for MSUD. Results may not be sufficient for newborns whose parents are both carriers. Special diagnostic testing should be performed in addition to newborn screening in this case.
- Test for high levels of leucine, isoleucine, and valine in plasma and urine.
- Genetic testing from blood (white blood cells) or skin (cultured skin fibroblasts) can help diagnose and help identify which type of MSUD a patient has.
- Molecular genetic testing for mutations in BCKDHA, BCKDHB, and DBT genes is used for prenatal diagnosis for at-risk pregnancies, to confirm the diagnosis of MSUD, and for carrier testing in at-risk relatives.
How is MSUD treated?
It is important to understand that, if not treated aggressively, MSUD can be fatal. Even a minor illness can cause a metabolic crisis in children with MSUD. Parents should call their child’s doctor immediately if they notice the child has extreme lethargy, low energy, poor appetite, personality or behavioral changes, vomiting, fever, walking/balance problems, or any sign of infection or illness.
Lifelong treatment with a special MSUD diet must be strictly followed to avoid episodes of metabolic crisis. A protein-restricted diet is necessary to avoid foods high in BCAAs. Foods to be avoided include cow’s milk, regular baby formula, eggs, cheese, meat, fish, nuts, dried beans, peanut butter, and regular flour.
For newborns and young infants, it is important to use a special medical baby formula that lacks BCAAs as a substitute for milk or regular baby formula.
Thiamine (vitamin B1) supplements can help patients with thiamine-responsive MSUD.
Regularly scheduled blood tests to tracking the BCAA levels of MSUD patients will be necessary so that diet and/or medical formula can be adjusted based on test results.
The BCKAD enzyme that is needed to break down BCAAs leucine, isoleucine, and valine is synthesized in the liver. Liver transplants have resulted in patients that are symptom-free and able to eat normal foods. However, this requires a major, high-priced surgical procedure and transplant patients must take expensive anti-rejection drugs for the rest of their life.
What is the prognosis for someone with MSUD?
There is no cure for MSUD. Treatment is lifelong and must be strictly followed. Patients that follow the strict MSUD diet and avoid illness and stress can manage the disease and grow into adulthood. If a metabolic attack occurs, it is crucial that MSUD patients seek immediate medical attention.
Other names for MSUD
- Branched-chain ketoacid dehydrogenase deficiency
- Branched-chain ketoacidurina
- BCKD deficiency or BCKAD deficiency

Great blog, Dawn! We’re starting clinical chemistry with the new class next week, and this will be great to share with them!
Thanks so much, Tracy! I’m so happy you have taken such an interest in Med Lab Study Hall. It is so nice to collaborate with someone that shares my passion for the medical laboratory professions. Your contributions to our website are invaluable!