When a person goes into the hospital they expect to get treated for their ailment and leave in a better position than when they came in. If infection control protocols are lax at a particular facility it is, unfortunately, possible for a patient to leave the hospital worse off than when they came in. With the emergence of superbugs due to the overuse/misuse of antibiotics the patient may become infected with a multidrug-resistant organism (MDRO).
The microbiology lab plays a very important role in infection control in the hospital with the main role being identification of pathogenic organisms. The lab also helps in data storage, epidemiological information, and appointing a representative to sit on the infection control committee. In order to better understand the micro lab’s role in infection control, we will take a look at the common types of hospital-acquired infections (HAIs), common etiologic agents, and finally the role the laboratory plays in the infection control process.
Common Types of HAIs
Before we look at the laboratory’s role in infection control, let’s take a look at some of the common types of Hospital Acquired Infections (HAIs). HAIs are the kinds of infections that the clinical microbiology lab assists in identifying and preventing.
Central Line Associated Blood Stream Infection (CLABSI)
CLABSI infections are bloodstream infections that develop from the central line and aren’t associated with any other infection at any other sight. To be considered a CLABSI the infection has to develop within 48 hours of central line placement. These infections can develop when proper protocols for insertion are not followed or when the line becomes contaminated during a routine procedure such as administering medication.
Catheter Associated UTI (CAUTI)
The cause of a CAUTI should be pretty self-explanatory. These infections are caused when a catheter is inserted into the urinary tract to aid in bladder drainage when a patient is not mobile. It is very important that all proper hygiene practices be followed when inserting the catheter to prevent exposure to pathogens. Clinical staff should also closely monitor the patient for symptoms of UTI and remove the catheter as soon as it is no longer needed.
Surgical Site Infection (SSI)
Surgical site infections are infections that occur after surgery at the sight that the surgery took place. These infections are rarely caused by negligence of medical staff or contamination. These infections are more often than not caused by the patient’s own normal microbial flora that becomes introduced to the site.
Ventilator-Associated Pneumonia (VAP)
Ventilator-associated pneumonia occurs when a patient is intubated and on a ventilator for a prolonged period of time. Typically, bacteria enter the patient’s lungs through the ventilator tube and causes an infection in the patient’s lung tissue. This type of pneumonia is common in patients in the ICU.
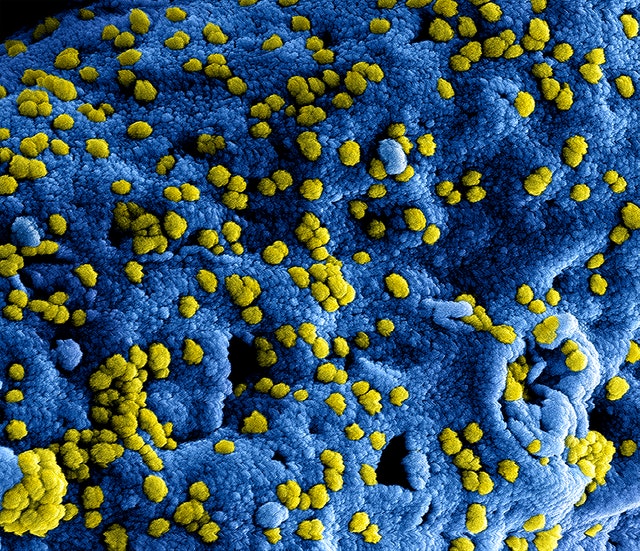
Common Etiologic Agents
The agents listed below are some of the common causes of HAIs. Bacteria continue to mutate and develop increasing resistance to stronger antibiotics, which increases the difficulty of treating these infections. It is better to contain these difficult-to-treat organisms to keep community spread to a minimum. Let’s take a look at some of the unique characteristics of each organism.
C. Diff
Clostridium difficile, or C. diff, is a gram-positive, anaerobic bacteria that can cause major complications should a patient’s GI tract become infected. The most vulnerable patients are those that are already immunocompromised or those that have received heavy antibiotic therapy for a previous infection. When an individual is immunocompromised, whether it be from a pathologic state or antibiotic usage, the individual’s gut flora becomes disrupted and allows for the overgrowth of C. diff. This can cause major gastrointestinal issues and is often very difficult to treat because C. diff naturally forms spores, making the bacteria resistant to most antibiotics.
An organism that is referred to as an ESBL is a gram-negative bacteria in the Enterobacteriaceae category that produces an enzyme called extended-spectrum beta-lactamase. This enzyme breaks down penicillins and cephalosporins and effectively renders the bacteria resistant to these types of drugs thus limiting the types of antibiotics that can be used to treat patients. ESBL organisms can affect a wide range of people and it is not uncommon that these types of infections develop in otherwise healthy individuals.
MRSA stands for methicillin-resistant Staphylococcus aureus. These strains of S. aureus are resistant to all beta lactam agents and are very difficult to treat. Like ESBL organisms MRSA can affect healthy individuals and be acquired in the community. Activities in which people are in close contact with each other help facilitate the spread of this organism.
Carbapenem-resistant Enterobacteriaceae are gram-negative bacteria that produce enzymes called carbapenemases. These enzymes inhibit the activity of carbapenems, cephalosporins, and penicillins. The population most at risk for developing this kind of infection are patients that have been hospitalized and those that have been treated with heavy doses of antibiotics
Vancomycin resistant enterococcus are enterococci that are resistant to vancomycin. This type of organism usually affects patients that have been hospitalized for a prolonged period of time, treated with heavy doses of antibiotics or are immunocompromised.
C. auris
Candida auris (C. auris) is a relatively new HAI. It is an infection caused by a yeast that is resistant to most of the typical antifungals used in healthcare settings. This particular organism generally affects those patients that have been hospitalized for a prolonged period of time, received heavy doses of antibiotics, or are immunocompromised.
Laboratory’s Role
Hospital-acquired infections are interconnected. Being infected with one type of organism can give rise to another type of infection. Example: A patient is on a heavy dose of antibiotics and not only do they develop a C. diff infection because of this but the heavy dose of antibiotics can cause bacteria to mutate and now the patient is also battling an infection with an ESBL organism. Microbiology plays an absolutely crucial role in maintaining this delicate balance.
Technical/Identification
The most important role that the microbiology lab plays in infection control is the identification of the pathogenic organism and performing a MIC to determine antibiotic sensitivity. This is what the infection control department of the hospital uses to determine when to isolate a patient and if there is an outbreak in a particular area of the health care facility. The antibiotic resistance results that the microbiology laboratory generates are also used by the pharmacy department to develop an antibiogram that is used to treat the patient and help prevent the development of further antibiotic resistance.
Infection Control Committee/Clinical Liason
A representative from the microbiology lab usually sits on the infection control committee in the hospital. This person acts as a liason between the laboratory and other departments of the hospital. The microbiology representative needs to effectively communicate the meaning of the microbiology laboratory results to other hospital departments and work as a team member to figure out why/how to contain an outbreak.
Environmental Cultures
The microbiology department is also responsible for culturing specimens obtained from the environment. This could range from anything including hospital tap water, swabs from frequently touched surfaces and medical instrumentation. The purpose of these cultures is two-fold:
1. Monitoring
The purpose of monitoring is to try and stop an outbreak before it starts. This will help determine how well a particular department is cleaned and how well staff adheres to standard precautions.
2. Outbreaks
Cultures are done in this scenario after an outbreak has already occurred. The purpose of performing environmental cultures in this situation is to determine how/why the outbreak occurred.
Monitoring for Unusual Cultures
Monitoring for unusual cultures entails a few things.
Agents of Bioterrorism – The microbiology lab screens for agents of bioterrorism and alerts the proper health authorities
New Antibiotic Resistance Patterns – The microbiology lab keeps track of antibiotic resistance and alerts infection control as to any unusual resistance patterns (e.g., an abnormal amount of pseudomonas resistant to imipenem).
Cultures growing unusual flora – The microbiology lab identifies and alerts appropriate departments when bacterial flora not usually affiliated with a particular body site is growing (e.g., yeast in a stool culture).
Device Contamination
The microbiology laboratory is responsible for culturing medical devices when contamination is expected. This directly detects infections such as CLABSIs and CAUTIs. These devices should be completely sterile and any growth is considered significant.
Data collection
Data collection happens in two main ways:
Storage of isolates – Isolates from blood cultures, CREs, MRSAs, VREs, and ESBLs are typically saved. Other types of isolates may be saved as per the request of the local health department.
Epidemiologic information – Reports for specific isolates are typically reported to the infection control committee. The locations of infections are also monitored to ensure a specific area is not experiencing an outbreak.
Potential Problems
Detection of organisms can take 24-72 Hours
Microbiology is slow work. When a culture comes into the lab it must be plated and incubated for 18-24 hours. The next day, the microbiology technologist determines whether any pathogenic bacteria are present. These bacteria are then set up on the laboratory’s identification system, typically means another 24 hours of waiting (exceptions being mid to large health systems that have state-of-the-art technology like MALDI-TOF).
If the isolated pathogenic bacteria is an ESBL, MDRO, VRE, or CRE, it needs to be confirmed by a second method. Depending on the method, it may add an additional 24 hours. So, all this together, that’s a total of 72 hours (longer if the culture is not pure and the pathogenic bacteria must first be isolated).
If the patient does not have a history of one of these problem bacteria, that means the patient has been in the general population for 3-4 days or even possibly discharged. During this time, the staff involved in that patient’s care could have inadvertently been spreading this very dangerous bacteria to others.
Lack of teamwork amongst departments
When an inpatient is infected with an MDRO, it is critical to isolate that patient from the general population residing on that floor. When an MDRO is identified in the lab, the first thing the technologist must do is call the inpatient floor to alert the clinicians. The clinicians then take charge of initiating isolation of the MDRO patient. Proper isolation involves several different departments, all of which are notified based on the action of the clinicians.
Let’s take a look at the following scenario. Suppose the clinicians forget to notify housekeeping to have them do a deep cleaning of the MDRO patient’s room upon discharge. The deep cleaning never gets done and a new patient gets moved into that room. Now, this new patient has been exposed.
Conclusions
Hospitals must remain vigilant in the infection control processes. Due to the overuse of antibiotics, emergence of new MDROs has become a huge problem. To try and control this the current strategy is to stop an infection before it starts, which means proper isolation of patients that have had infections with MDROs, proper cleaning of rooms where patients with MDROs reside, and of course proper identification of pathogenic organisms.