Introduction
We’ve all heard, time and again, the importance of electrolytes to help keep our bodies running like a well-oiled machine. Sodium, potassium, chloride, and bicarbonates are significant electrolytes, as well as phosphate, calcium, and magnesium.
Magnesium has many important functions in the body. Adenosine triphosphate (ATP) is the main source of energy for the cells in our body…and guess what? It must be bound to magnesium to be biologically active. So no magnesium = no cellular function. Magnesium is an important cofactor for over 300 enzymes in the body and is important in maintaining heart and neuromuscular function.
This blog will focus specifically on hypomagnesemia, which is a decreased level of magnesium in the blood.
Unfortunately, magnesium is often considered the forgotten electrolyte, primarily because patients rarely show symptoms of hypomagnesemia until levels are really low. In the general population, the reported incidence of hypomagnesemia is only approximately 2%. This is likely due to the aforementioned lack of symptoms until levels are very low. However, it is becoming a more widespread problem in hospitalized patients (12%), especially patients in intensive care units (as high as 60 – 65%). Below is a list of risk incidences from Mayo Clinic.
Recent Risk Incidences (Mayo Clinic)
- 2% in the general public
- 10% – 20% in hospitalized patients
- 50% – 60% in intensive care unit patients
- 30% – 80% in persons with alcohol use disorder
- 25% in outpatients with diabetes
Let’s take a look at how magnesium levels are maintained in the body.
Magnesium Homeostasis
The normal reference range for serum magnesium is 1.59 – 2.67 mg/dL. Because this reference range is so narrow, critical levels are reached quickly. Using the reference range of 1.59 – 2.67 mg/dL, a value of 1.5 mg/dL may be considered low and not given much attention by the clinician because it is just outside the reference range. However, let’s say that a level of 1.4 mg/dL may be considered a critical value for this particular laboratory. In this case, a magnesium value of 1.4 mg/dL requires immediate attention. (Note: Magnesium reference ranges and critical values may differ slightly across different clinical laboratories.)
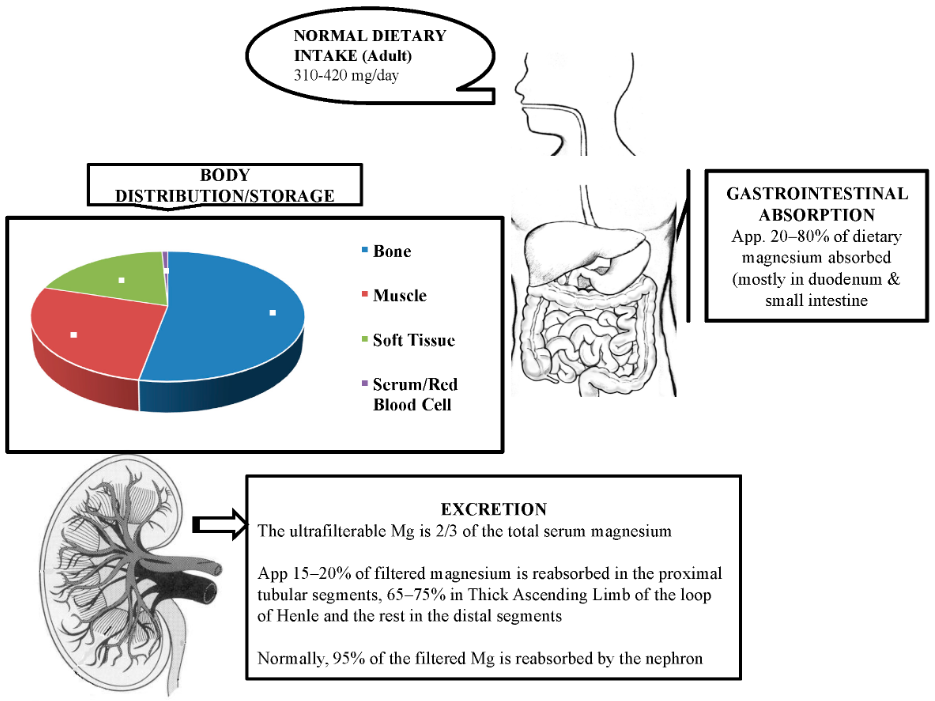
So how is magnesium regulated in the human body? Magnesium homeostasis depends on its absorption in the small intestine, storage in bone (largest distribution of magnesium stored in bone) and tissue, and its reabsorption and excretion by the kidneys (primarily involves the thick ascending loop of Henle, but also the proximal and distal tubule).
It is interesting to note that hypomagnesemia can also cause hypocalcemia; the two are interconnected. Hypocalcemia stimulates parathyroid hormone (PTH) release from the parathyroid glands, and PTH enhances intestinal absorption and kidney reabsorption of magnesium. So, PTH also helps maintain magnesium homeostasis.
Severely low magnesium levels can also cause hypokalemia (low potassium levels). Magnesium, calcium, and potassium levels must ALL be corrected to return to normal levels.
Distribution and Storage of Magnesium in the Body
Most magnesium in the body is in storage (around 99%), with the largest storage area being bone tissue. Less than 1% of magnesium is in serum and red blood cells. Serum magnesium is present in three states: ionized form (nearly two-thirds), bound to albumin (nearly one-third), and the tiny bit that is left is complexed to anions. Serum magnesium values that are analyzed in the clinical laboratory measure total serum magnesium.
What causes hypomagnesemia?
There are four processes that cause hypomagnesemia. They are:
- Decreased Dietary Intake,
- Gastrointestinal Loss,
- Renal Loss, and
- Redistribution from Extracellular to Intracellular.
Let’s take a deeper look at each process.
– – Decreased Dietary Intake
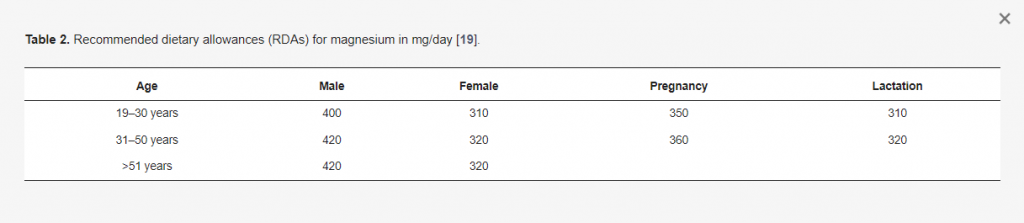
There are studies that estimate that nearly three-fourths of Americans do not have a diet that contains the recommended dietary allowance of magnesium. That is an astonishing estimate! However, even with an estimate that large, only about 2% of the general population is actually reported to have hypomagnesemia.
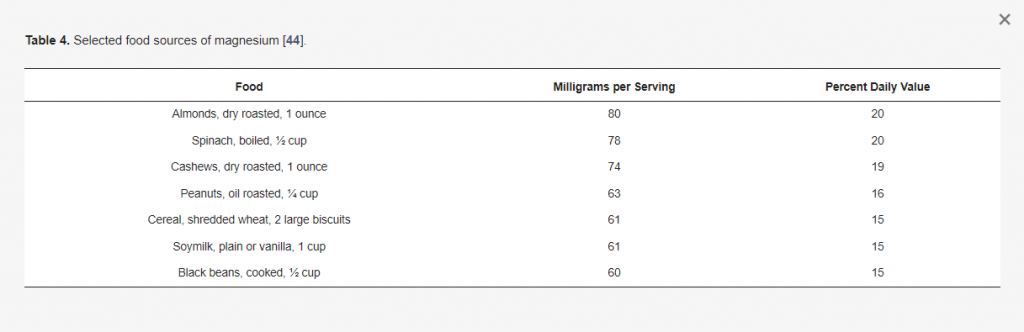
First and foremost, magnesium levels are affected by the overall dietary intake of foods from the different food groups, as well as foods that contain sufficient magnesium. Sources of dietary magnesium come from magnesium-rich foods, such as leafy green vegetables, nuts, seeds, legumes, and whole grains. If you are not getting the recommended dietary allowance of these essential foods, you may have acquired hypomagnesemia.
Hypomagnesemia can be secondary to decreased dietary intake. Examples of this are alcohol use disorder, starvation, and in patients who are critically ill patients that receive total parenteral nutrition (TPN) intravenously.
Low magnesium levels can also occur secondary to the use of certain medications. Examples are loop and thiazide diuretics that interfere with the transfer and reabsorption of minerals in the kidneys, proton pump inhibitors (PPIs) like Prilosec (omeprazole) and Nexium (esomeprazole) that interfere with absorption in the intestine, certain antibiotics (aminoglycosides and amphotericin B), digitalis (digoxin), and certain chemotherapeutic drugs (cisplatin and cyclosporine).
Here’s a fun tip and possibly an excuse to eat one of your guilty pleasures. Dark chocolate is an excellent source of magnesium! (Cue the marching band and confetti!)
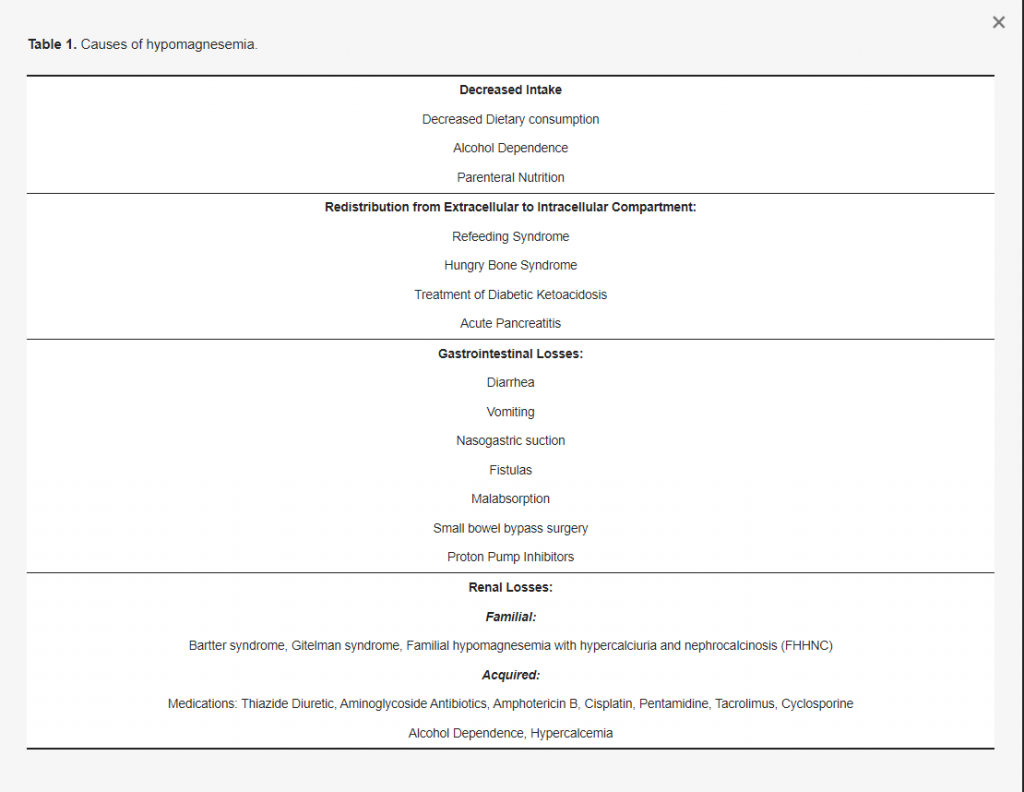
See the table below for hypomagnesemia caused by gastrointestinal loss, renal loss, and redistribution from extracellular to intracellular.
What are the symptoms of hypomagnesemia/How does it affect the body?
Symptoms of hypomagnesemia fall under the following categories: neuromuscular, central nervous, and cardiovascular. As mentioned earlier, symptoms may not actually occur until magnesium levels are significantly low.
| Neuromuscular | Central Nervous | Cardiovascular |
| Fatigue | Decreased reflexes | Cardiac arrhythmias |
| Muscle weakness | Confusion | High blood pressure |
| Twitching (fasiculations) | Abnormal eye movement | Heart palpitations |
| tetany | Mental health conditions – apathy; increased risk of depression | Increased risk of heart failure – magnesium deficiency causes decreased potassium in heart muscle cells |
| Convulsions | Bradycardia |
Other symptoms include loss of appetite, nausea, vomiting, weakened bones.
Remember that decreased magnesium levels can also lower potassium and calcium. It is not certain whether the cause of weakened bones is due to decreased magnesium alone or whether it only occurs when the calcium levels decrease.
Severely decreased magnesium levels can have life-threatening or fatal complications such as:
- Cardiac arrythmias
- Seizures
- Coronary artery vasospasm
- Ventricular arrythmia
- Sudden death
- It is also associated with increased mortality and prolonged hospitalization.
How do we test for magnesium in the clinical laboratory?
- Total magnesium is measured on serum, heparinized plasma (sodium heparin or lithium heparin), or urine (both random and 24-hour). If unable to determine whether the cause of hypomagnesemia is due to renal loss or GI loss, measure 24-hour urinary magnesium excretion. In addition, fractional excretion of magnesium can be calculated on a random urine sample magnesium level using this formula:
[(UMg x PCr) / (PMg x UCr x 0.7)] x 100
* U and P refer to the urine and plasma concentrations of magnesium (Mg) and creatinine (Cr) * - If the patient has normal renal function tests and fractional excretion of magnesium is >2% = hypomagnesemia is considered secondary to renal magnesium wasting from drugs such as diuretics, aminoglycosides, or cisplatin.
- SERUM REFERENCE RANGE: 1.59 – 2.67 mg/dL
- URINE REFERENCE RANGES:
- 24-hour urine collection:
- Adults: 6-10 mEq/day (3-5 mmol/day)
- Random urine:
- Male, <40 yr: 2.1-23.2 mg/dL (0.86-9.54 mmol/L)
- Female, <40 yr: 1.2-18.7 mg/dL (0.49-7.69 mmol/L)
- Random urine:
- Male, ≥40 yr: 0.6-13.7 mg/dL (0.25-5.63 mmol/L)
- Female, ≥40 yr: 0.4-15 mg/dL (0.16-6.17 mmol/L)
- Male: 18-110 mg/g creatinine (0.74-4.53 mmol/g creatinine)
- Female: 14-139 mg/g creatinine (0.58-5.72 mmol/g creatinine)
- 24-hour urine collection:
- Testing can be challenging because magnesium tends to collect in bone and tissues, not blood.
- Sources of error:
- hemolysis – may be falsely elevated;
- cannot use oxylate, citrate, or EDTA anticoagulants.
How is hypomagnesemia treated?
- Asymptomatic patients can be treated as outpatients with prescribed sustained-release oral magnesium supplements. These should be tried first and .
- Symptomatic patients should receive parenteral supplements and may need to be admitted. Speaking from personal experience, IV therapy can be given as an outpatient in a designated infusion therapy site where treatment and vitals can be monitored by nursing personnel and where a physician can be easily obtained in case of an emergency.
- Serum magnesium levels rise quickly after treatment and levels must be rechecked to ensure effective treatment. Keep in mind that intracellular magnesium takes longer to be replenished.
- Magnesium supplements – usually given via IV when levels are severely low. Magnesium oxide or magnesium citrate can be taken in pill form. However, one review did find that magnesium supplements are not an effective treatment for muscle cramps in older adults.
- Magnesium rich foods such as seeds and nuts (almonds, pumpkin seeds, oats, etc.), whole grains, legumes, and leafy green vegetables. Many breakfast cereals have magnesium added.
- Need an excuse for chocolate addictions? Dark chocolate is a good source of magnesium!
- If loss is due to renal loss, amiloride (a potassium- and magnesium-sparing diuretic) can be prescribed.
- Patients taking PPIs should consider switching to alternative medical treatments. One example is switching from omeprazole (PPI) to famotidine (non-PPI).
- Magnesium sulfate is the drug of choice for treating eclampsia in pregnant women.