Immunity, by simple medical definition, is the process that occurs to protect the body against pathogens and infectious diseases. There are various processes within our body that are part of the immune response, including inflammation, phagocytosis, antibody synthesis, and the activation of the complement system.
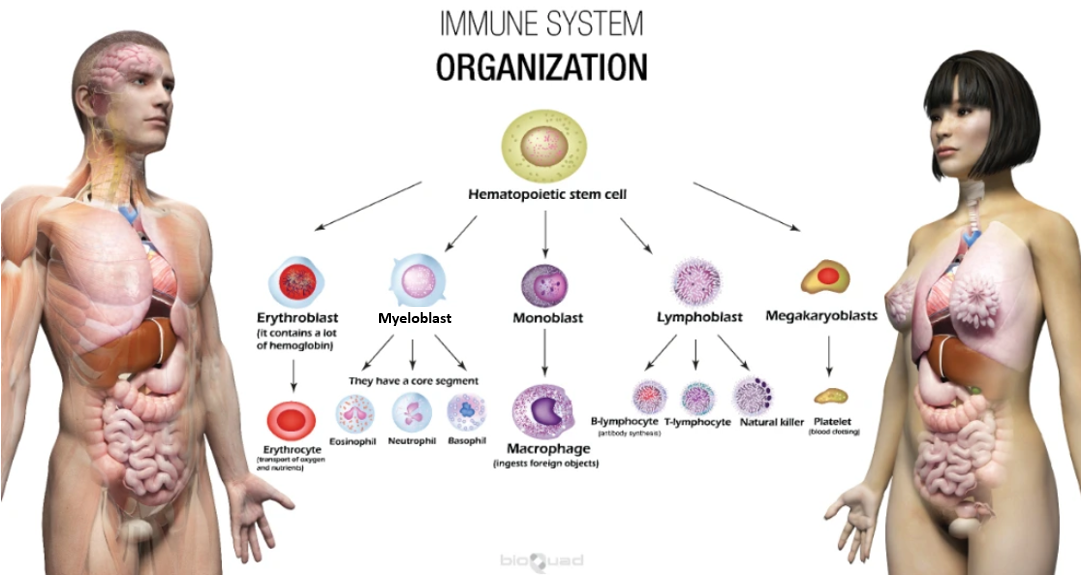
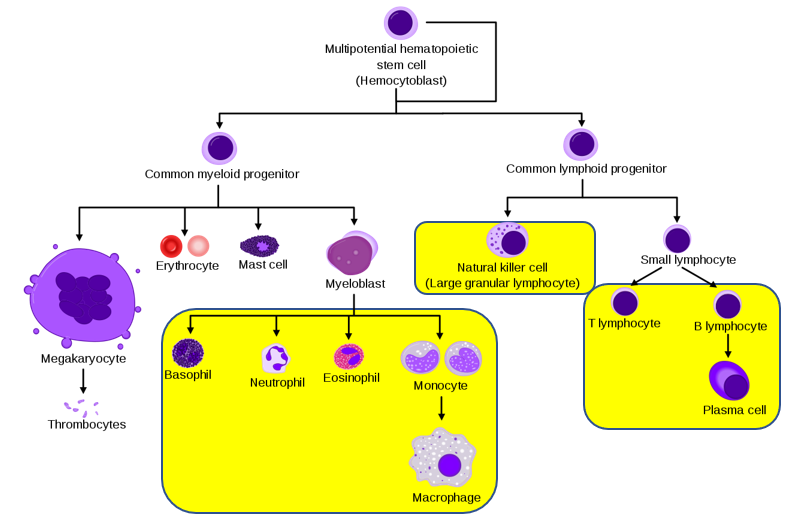
Our immune system is very reliant on white blood cells (leukocytes) from both the myelocytic and lymphocytic lines of leukocytes. The myelocytic line of leukocytes participates in inflammation and phagocytosis (innate immunity). The lymphocytic line is more involved in cellular- and humoral-mediated immunity (acquired immunity).
The yellow highlighted areas on the image below show the primary cells involved in our immune system. In addition to those marked in yellow, there are other cells that assist in the immune response. These are dendritic cells, mast cells, and Langerhans cells (dendritic cells found specifically in the skin).
Let’s take a look at the two types of immunity: innate immunity and acquired immunity.
Innate Immunity (also known as nonspecific immunity or natural immunity)
Innate immunity allows us to respond to and resist foreign microorganisms because of cells and cellular functions that already exist in the human body. We are born with these and do not need to have prior exposure to the foreign invader for the action to occur. Actions are the same no matter what type of pathogen or foreign material invades the body.
The first line of defense of the innate immune system attempts to keep microorganisms out of our body. This includes physical barriers such as the epithelial cells of our intact skin and mucus membranes in our nose and mouth that help trap microorganisms. Chemicals that are secreted by cells and tissues are another first line of defense. These include things such as the acidic pH of our skin surface, saliva, breast milk, lysozymes found in tears, and many others.
The second line of defense includes the processes of inflammation and phagocytosis, as well as activation of the complement system. Inflammation causes a response that recruits neutrophils and macrophages to sites of infection. These cells are the primary line of defense in the innate immune system. Below is an image and description of what occurs in the innate immune system when bacteria invade our body.
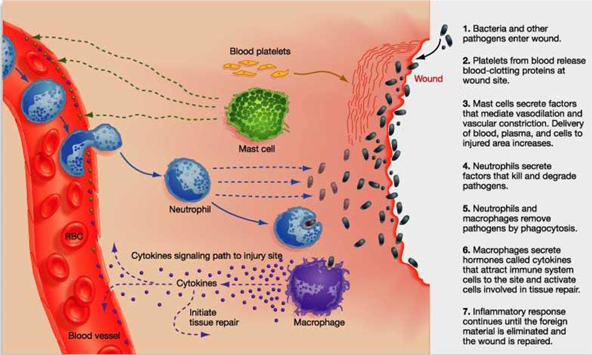
The peripheral blood leukocytes that are part of the innate immune system are neutrophils, eosinophils, basophils, and monocytes. Neutrophils are the most abundant, comprising 40-60% of all leukocytes in the blood. Nearly half of the neutrophils adhere to arteriole and capillary walls so they can easily move to the tissues to fight foreign intruders. The process of adhering to the vessel walls is known as margination and the process of squeezing through the blood vessels is called diapedesis.
Invaded areas release chemical messengers that entice cells to leave the bloodstream. These chemical messengers are known as chemotaxins and the movement of cells toward the chemotaxins is known as chemotaxis. Of these leukocytes, the monocytes spend a relatively short time in circulation, then migrate to the tissues and become macrophages.
Monocytes comprise 2-8% of all leukocytes in the bloodstream. What monocytes lack in quantity they make up in size and phagocytic ability. These cells transform into macrophages once they leave the bloodstream and each macrophage can engulf a lot of foreign organisms.
As far as eosinophils (1-3% of circulating WBCs) and basophils (0-1% of circulating WBCs), these cells are mostly involved in allergic responses. Eosinophils are also responsible for fighting multi-cellular parasites.
The complement system is a series of 20+ proteins that, once activated, stimulate the inflammatory response, enhance phagocytosis, and lyse foreign intruders.
Acquired Immunity (also known as adaptive immunity or specific immunity)
Acquired immunity occurs only after someone encounters a specific challenge and the immune system responds specifically to that challenge. It develops when someone’s immune system actively responds to a foreign antigen or occurs after someone passively receives antibodies from another source. The cells involved are lymphocytes and plasma cells.
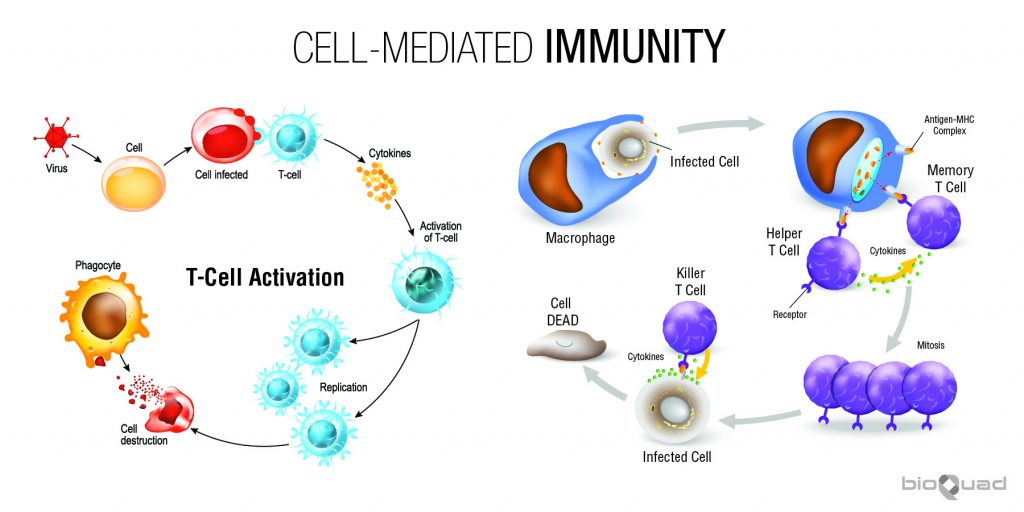
There are two types of immune responses in adaptive immunity: cell-mediated immunity and humoral-mediated immunity.
Cell-mediated Immunity
Cell-mediated immunity is an immune response that does not involve antibodies. Rather, cell-mediated immunity is the activation of phagocytes, antigen-specific cytotoxic T-lymphocytes, and the release of various cytokines in response to an antigen.
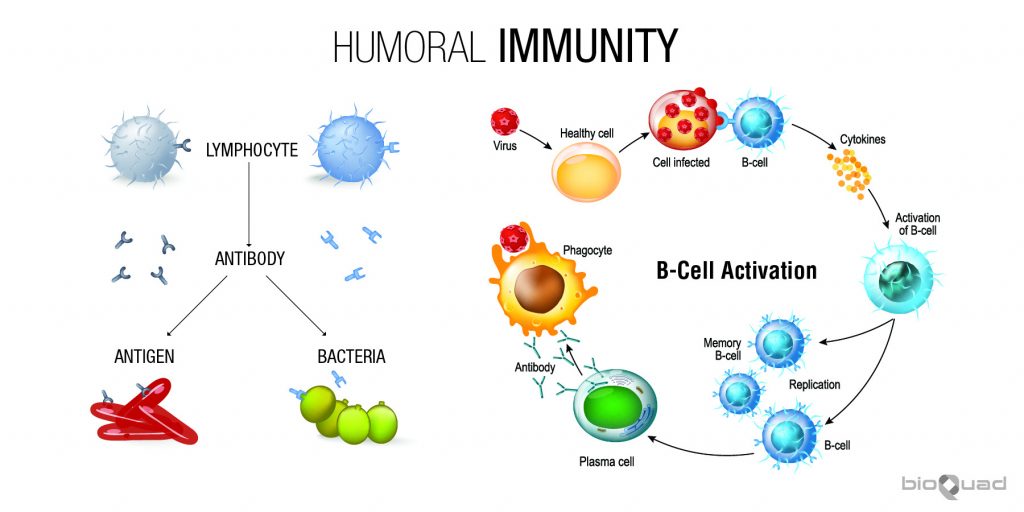
Humoral-mediated Immunity
Humoral immunity is also called antibody-mediated immunity. With assistance from helper T cells, B cells will differentiate into plasma cells, which produce antibodies against a specific antigen. The humoral immune system deals with antigens from pathogens that are freely circulating, or outside the infected cells.
Acquired immunity can be obtained either actively or passively. If obtained actively, the immunity is long-lasting. If obtained passively, the immunity is only short-term. Let’s take a more detailed look at how active and passive immunity are acquired.
↠ Active Immune Response
Active immunity occurs when we are exposed to the actual disease-causing organism, triggering our immune system to produce antibodies to that specific disease. A disease-causing organism (antigen) that elicits an immune response is referred to as an immunogen. There are two (2) types of active immunity: natural active immunity and artificial active immunity (also called vaccine-induced active immunity).
- Natural Active Immunity – Acquired from having an actual infection with a disease through exposure to that disease. For example, your child goes to her best friend’s weekend birthday party. When your child returns to school on Monday she notices that her best friend is not there, and later finds out that the best friend has chickenpox. About two weeks later, your child has chickenpox. She develops her own antibodies to chickenpox and becomes immune to getting that disease again.
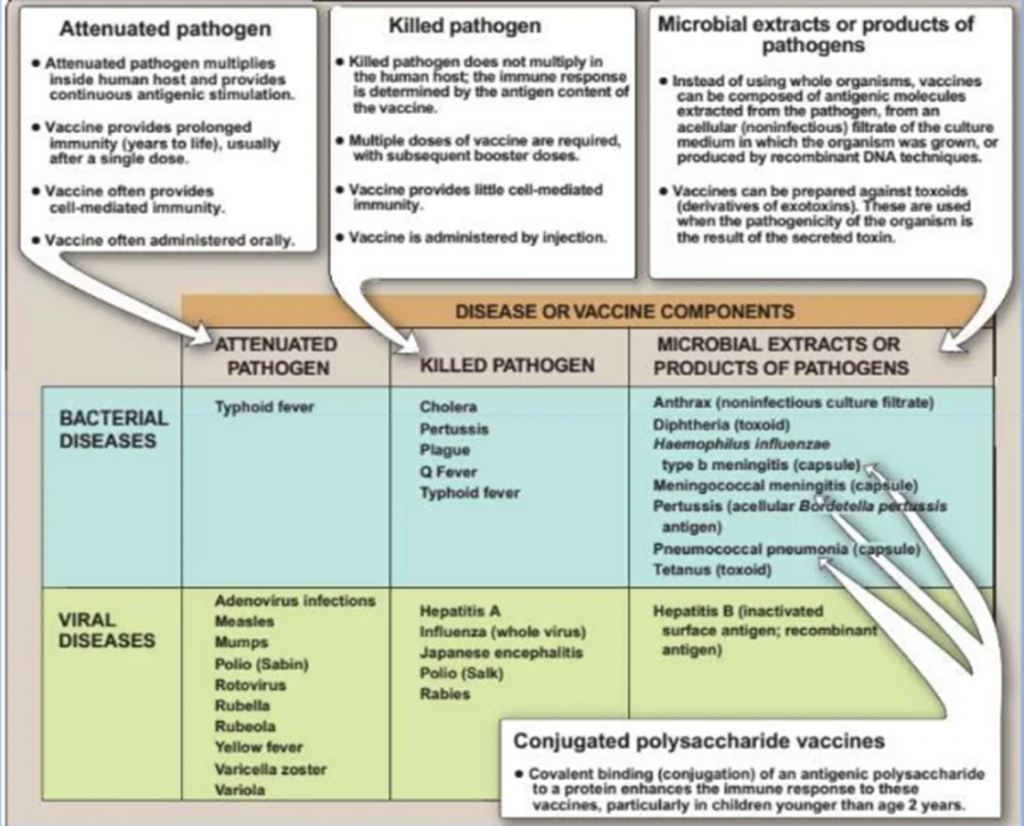
- Artificial Active Immunity (Vaccine-induced Active Immunity) – Acquired through vaccination with a killed or weakened (attenuated) form of a disease organism. For example, your child has the chickenpox vaccine and develops antibodies to chickenpox, becoming immune to that disease. Below is a chart depicting artificial active immunity.
Whether natural or artificial (vaccine-induced), active immunity is long-lasting and often lifelong. Whenever contact with that disease happens in the future, your immune system will recognize it and immediately begin producing antibodies to destroy it.
↠ Passive Immune Response
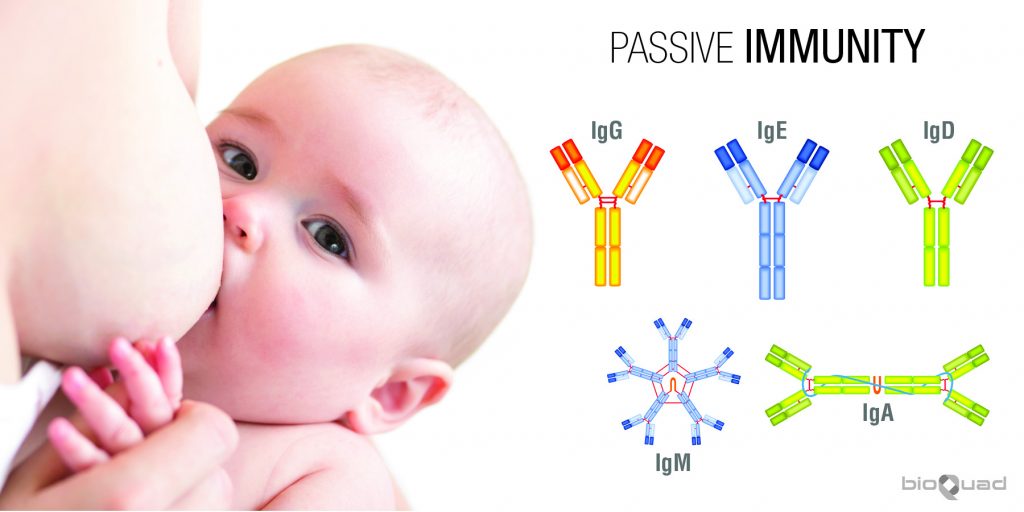
Rather than producing antibodies through their own immune system, non-immune individuals are given preformed antibodies that were produced in another person or animal. This only provides short-term immunity (3-6 months) and is typically used when there is a very high risk of infection and not enough time for the body to develop and activate its own immune response. Immediate protection is provided but it is temporary. There is the risk of being infected with the exact same pathogen later, which means the patient does not develop memory of the previous exposure. This type of immunity can be natural or artificial.
- Natural passive immunity is the transfer of maternal IgG antibodies to the fetus through the placenta or IgA antibodies through breast milk and colostrum (the first maternal breast secretions). These IgG antibodies protect the newborn against any pathogens to which the mother has developed immunity, either through natural infection or through vaccination. This type of immunity provides infant protection during the first few months of life, while their own immune system is developing.
- Artificial passive immunity entails the administration of antibodies that are specific for a pathogen or toxin to non-immune individuals. This provides short-term protection and is administered in several forms.
- Human Immune Serum Globulin (HISG) – Immunocompromised patients have had HISG administered for many years. This consists of predominantly IgG antibodies for numerous antigens in an attempt to provide indiscriminate humoral protection against a potpourri of pathogens. HISG is prepared from treated, pooled serum of many donors (in the U.S., these donors must first test negative for hepatitis B and HIV in the U.S.).
- Antigen-specific Immune Globulin (hyper-immune globulin) – This uses pooled human serum from individuals that have developed immunity against a specific pathogen (either through infection or vaccination). It is used to treat non-immunized people who have potentially been exposed to that specific pathogen. Some of these have been prepared from animal sera, typically horse serum, and have had good results. Examples include antisera against snake venom, and antitoxins for diphtheria, tetanus, and botulism. (NOTE: There is some risk of anaphylactic shock, as sometimes antibodies from other animals are seen as foreign.)
- Monoclonal Antibodies – These are man-made proteins that act like actual human antibodies. They are derived by cloning a single B cell that targets an exact location on a specific antigen and then produced in large quantities. Monoclonal antibodies are used to treat many diseases, including some types of cancer.
Summary
Innate or Acquired? If acquired, is it obtained actively or passively? Even though this has been a brief introduction to immunity and the immune response, the information presented may seem a bit daunting. So let’s look at a quick snapshot of what we’ve learned.
Innate Immunity
- Non-specific; natural.
- Includes physical and chemical barriers (epithelial cells, mucus, acid pH of skin, lysozymes, complement).
- Involves inflammation (vasodilation, margination, diapedesis, chemotaxis) and phagocytosis (neutrophils, monocytes become macrophages – antigen-presenting cells), and the complement system.
Acquired Immunity
- Specific; adaptive
- Cells involved are lymphocytes and plasma cells
- Cell-mediated or Humoral
- Active – long-term protection (exposed to antigen; can be natural = infection organism itself or artificial = attenuated organism vaccine)
- Passive – short-term protection (exposed to antibody; natural = through placenta IgG or breast milk IgA or artificial = injection (pooled gamma-globulin, monoclonal Ab)
We hope this has been a helpful introduction to immunity and the immune response. Please be sure to check back each month for more exciting medical laboratory-related blogs!