What are cardiac biomarkers and why do we use them?
In the clinical laboratory, evaluating sudden onset chest pain and shortness of breath includes analyzing cardiac biomarkers. Ideal biomarkers are specific to the heart tissue, would be detectable early in the onset of symptoms, and offer a trending pattern that can be interpreted as symptoms progress or digress.
We’ll discuss two cardiac biomarkers here: Troponin and B-type natriuretic peptide (BNP).
The American College of Cardiology recommends using Troponin for diagnosing acute myocardial infarction (AMI, also known as a heart attack) in the emergency department (www.acc.org).
B-type natriuretic peptide is used to diagnose heart failure (also known as congestive heart failure or CHF).
Both biomarkers may be used to risk-stratify patients and predict patient outcomes during treatment. Prognostic evaluation and risk stratification are beyond the scope of this discussion.
Troponin
The troponin complex is an integral part of cardiac muscle fibers and consists of 3 subunits: Troponin I, Troponin T, and Troponin C. When muscle fibers are relaxed, the troponin complex covers the binding sites for myosin and keep the muscle fiber from contracting.
When the cardiac muscle cells (cardiac myocytes) receive a signal from the nervous system, the sarcoplasmic reticulum inside the myocytes opens calcium channels and dumps a large amount of calcium into the cytoplasm.
Troponin C binds this free calcium and causes the troponin complex to change shape. This new conformation of the troponin complex exposes the binding sites for myosin, which attaches to the muscle fiber and induces muscle contraction.
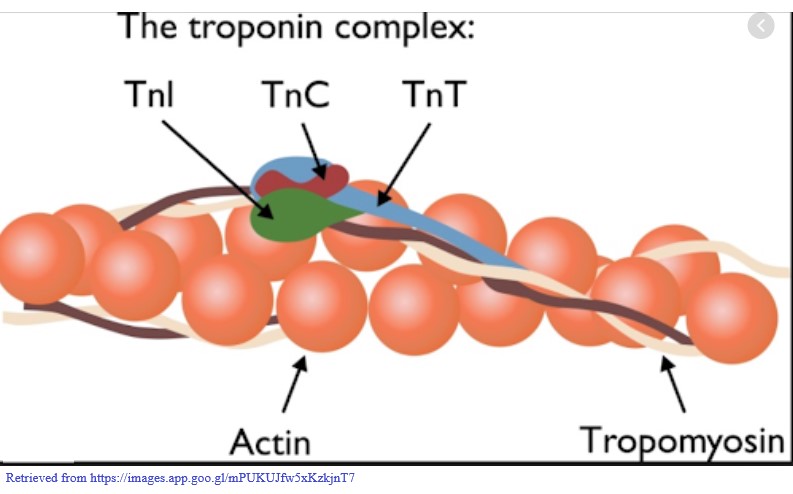
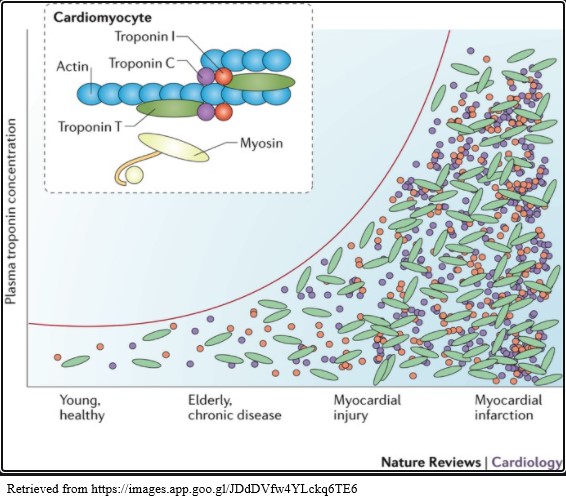
When damage to the cardiac myocytes occurs, such as during an acute myocardial infarction and/or heart failure, the muscle fibers degrade and release the Troponin subunits into the bloodstream.
Troponin Reference Ranges
Troponin levels less than 0.04 ng/mL indicate no heart damage has occurred.
Levels greater than 0.40 ng/mL indicate a probable AMI has occurred, and should be evaluated with other indicators such as an electrocardiogram and patient symptoms.
Levels from 0.04 – 0.39 ng/mL indicate some type of heart damage is occurring that is probably not an AMI, possibly heart failure (www.medicalnewstoday.com).
Troponin and AMI vs CHF
Troponin levels are detectable in the blood stream as early as 2 hours after a myocardial infarction occurs and remain detectable for 7-10 days (www.emedicine.medscape.com). This allows rapid diagnosis of an acute infarct as well as detection of an older infarct if the patient does not present to the emergency department immediately after symptom onset.
Especially with women, a trip to the emergency department may be delayed because symptoms of myocardial infarction are not the typical pain and tightness in the chest. The most frequent symptoms for acute MI in women are shortness of breath, weakness, and fatigue – which can be associated with many other conditions, making it difficult to quickly identify AMI in women.
If you experience these symptoms, seek a medical professional. If they progress to classical AMI symptoms, call 911. It is the fastest way to get treatment before the heart is beyond saving and causes death.
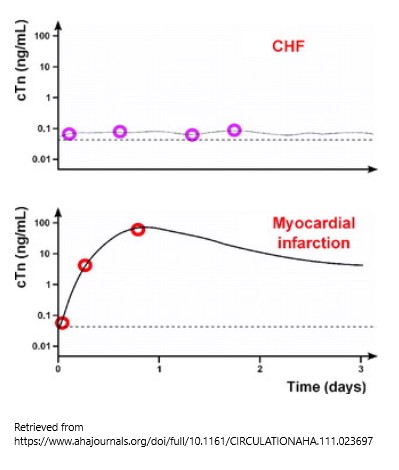
During heart failure (CHF), Troponin leaks at a constant low level, without the rapid rise that is seen with AMI. Troponin alone should not be used to diagnose and monitor heart failure, however. The recommendation is to use BNP for heart failure diagnosis.
B-type Natriuretic Peptide (BNP)
BNP is one of the natriuretic peptide hormones that affect the circulatory system. BNP is produced by the ventricles of the heart when the heart muscle is stretched as a result of heart failure and hypertension (www.health.harvard.edu).
The muscle stretching is caused by the weakened heart muscle’s inability to push the blood through from the ventricles. Incomplete evacuation of the ventricles causes fluid backup and retention throughout the body.
BNP Function, Reference Range & CHF
BNP is produced in an effort to reduce blood pressure due to the increased blood volume by dilating the blood vessels. It also acts on the kidneys to increase salt and water excretion to reduce the amount of fluid in the circulation. The final outcome of BNP production is to reduce the amount of work the heart needs to do to push the blood through the circulatory system.
When diagnosing congestive heart failure (CHF), BNP levels of 0-100 pg/mL rule out the condition. As the level of BNP increases, the severity of the condition increases.
BNP & CHF Treatment
Prognostically, if treatment can reduce the backup of blood into the heart and allow the ventricles to return to a smaller size, the BNP will decrease indicating that the treatment is working. If treatment fails, BNP production will continue due to the stretching of the ventricles and will continue to rise or remain elevated.
BNP may also increase in noncardiac conditions (kidney failure, liver disease, brain hemorrhage). Therefore additional testing such as electrocardiogram, echo sonography of the heart, or other laboratory tests may be needed to rule out noncardiac conditions.
In Summary
Diagnosis of acute and chronic heart damage can be aided by laboratory tests such as Troponin and B-type natriuretic peptide.
Rapid diagnosis is critical for AMI so that treatment can begin. Rapid treatment decreases the chance of extensive myocardial damage that could lead to death. Troponin is released by damaged heart muscle. It allows rapid diagnosis due to it being released as early as 2 hours from the time of the AMI. It also allows the diagnosis of an older MI because it remains elevated for several days after the MI has occurred.
BNP helps distinguish AMI from heart failure. It is produced in response to cardiac muscle stretching as it weakens without muscle damage or death, whereas Troponin is released from damaged or dying muscle.
Don’t Hesitate – Call 911
If you experience any symptoms of heart trouble, seek medical help. Call 911. Go to the emergency department and let the medical and laboratory professionals aid in your diagnosis. Your life may depend on your quick action.