You may have seen appeals by blood suppliers saying your donation can help save up to three (3) lives. I was recently asked how and why that happens. There are two main reasons.
Not every patient needs all the components in a unit of blood, so they are separated and the patient only receives the portion they need. In addition, different parts of the blood need to be stored at different temperatures to maintain the best function.
When you donate blood, you can see that there isn’t just one bag, but several bags attached to each other, as well as a filter. As blood leaves the donor’s arm, it is filtered to remove the white blood cells. It is collected in the main bag and sent to a blood center for processing.

Once at the blood center, it is put into a centrifuge to separate the red cells and plasma (the liquid portion of the blood). From these two components, all the other products can be obtained. These products include red blood cells (Packed Red Blood Cells – PRBC), plasma (Fresh Frozen Plasma – FFP), platelets, and cryoprecipitate (cryo).

Here is another type of collection that not many people have heard of: apheresis. In an apheresis collection, the tubing from the donor’s arm does not go to a bag, but to an instrument that can separate the blood, keep the portion they wish to collect, and return the rest to the donor. This method of collection can be used to collect red cells, platelets, and plasma. It is used most frequently to collect platelets and what are known as “power reds”, where two units of red cells are collected at one time.

Let’s talk about the different blood components and how they are stored and used.
Red Blood Cells (Packed Red Blood Cells – PRBC)
After being separated from the plasma, there may be an additive solution added to the red cells. The additive solution acts as a preservative. Depending on the anticoagulant used, and if there is an additive solution, red cells can be stored in a refrigerator (1-6∘C) for 28-42 days. If the donor has a rare blood type, the red cells can also be frozen in glycerol and kept for up to 10 years.

Red cells are transfused for a wide variety of reasons. Their function is to maintain oxygen-carrying capacity. They are given in cases of trauma and surgery, both of which may cause significant blood loss. There are also many types of anemia (low blood count) that are treated by transfusion if the patient does not respond to anemia medications. Iron deficiency, B12/folate deficiency, anemia due to a chronic disease, medication, or chemotherapy are all treated with red cell transfusion. Mechanical heart valves can cause increased destruction of red cells and cause anemia. Other disorders such as sickle cell disease and thalassemia require regular transfusions.
Platelets
Platelets are unique in that they are the only component stored at room temperature. Because of this, they are the most susceptible to bacterial contamination and have a life span of only five (5) days (which may be extended to 7 days under certain conditions). For patient safety, platelet donations are subject to additional testing for bacterial contamination.

Over 90% of platelets in the United States are collected by apheresis donations. The platelets are suspended in a mixture of plasma and platelet additive solution. Some platelets may also be treated with psoralen, which inactivates bacteria and viruses.
Platelets are used to prevent bleeding in patients who have either a low platelet count or platelets that do not function. Platelets can be consumed rapidly with active bleeding. Many patients undergoing chemotherapy do not make enough platelets and require transfusion. In cases of platelets disorders, or anti-platelet medications, the patient’s count may be normal, but the platelets themselves do not function.
Plasma (Fresh Frozen Plasma – FFP)
Plasma is frozen quickly after separation and stored at -18∘C for up to 1 year after collection. Before it can be transfused, it must be completely thawed in an FDA-approved 37∘C thawing device. If this device is a waterbath, the FFP unit must be placed inside a plastic bag to protect the ports on the unit. Once thawed, the FFP can be stored at 1-6∘C for 24 hours.

Plasma is transfused to correct coagulation abnormalities. Plasma contains all the factors needed to initiate the clotting process and control bleeding (except for platelets which are a separate component.). These factors can become depleted in active bleeding from trauma or gastrointestinal bleeding, or the patient may not be making enough coagulation factors due to liver disease, hepatitis, or alcoholism.
Plasma can also be used in exchange transfusions. The apheresis machine is used to remove the patient’s plasma while transfusing fresh plasma from donors. This is used to treat a condition called thrombotic thrombocytopenic purpura (TTP), a rare blood disorder that causes small clots throughout the body. It can also be used to lower the amounts of antibodies in the patient and treat autoimmune disease.
Plasma also contains antibodies of the donor. During the Covid pandemic, patients were given plasma containing Covid antibodies to attempt to speed recovery. For more information, check out our blog from July 2020 on Covid-19 Convalescent Plasma.
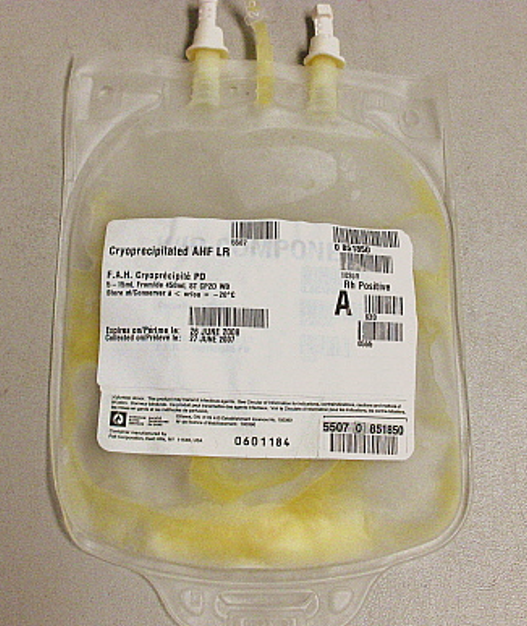
Cryoprecipitate
Cryoprecipitate (cryo) is an insoluble protein that contains fibrinogen, von Willebrand’s factor, and other clotting factors. Fibrinogen is the protein that makes fibrin, the main substance that makes a clot. Cryo is made from plasma by thawing it slowly at 1-6∘C. The protein is separated by centrifugation, suspended in a small amount of plasma, and refrozen. It can be stored up to one (1) year from the date of collection at -18∘C. It is given when a concentrated source of fibrinogen is required, typically for heart surgery, trauma, and other cases of extreme blood loss.
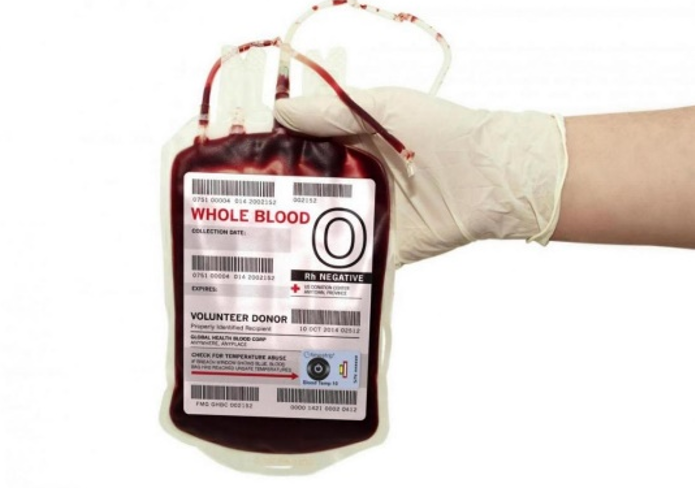
Whole Blood
Whole blood has not separated into its various components, but left “whole”. It is not used frequently but can be used in cases of trauma when the patient is losing a large volume of blood. Whole blood is sometimes used during transport by ambulance or helicopter to try and stabilize the patient until they can arrive at the hospital.
In Conclusion
By separating the components of blood, each portion can be stored at the correct conditions to optimize its function when transfused, and allow each patient to receive only what they need. One whole blood donation can potentially save up to three (3) lives. If you are able, please consider donating blood as often as possible.

