When you first learn about blood types, it seems pretty easy. There are 4 types: O, A, B, and AB. But once you’ve learned that, you find that it isn’t all black and white.
One of the most common complications encountered in Blood Bank is the ABO discrepancy, where the forward type (or front type) indicates one ABO blood type and the reverse type (or back type) indicates a different ABO blood type. This has to be resolved before type-specific blood can be given to the patient. This blog discusses the most common discrepancies and how to investigate and resolve them.
But first…a primer on ABO blood types, Landsteiner’s Rule, and forward and reverse blood typing
ABO Blood Group Antigens & Antibodies
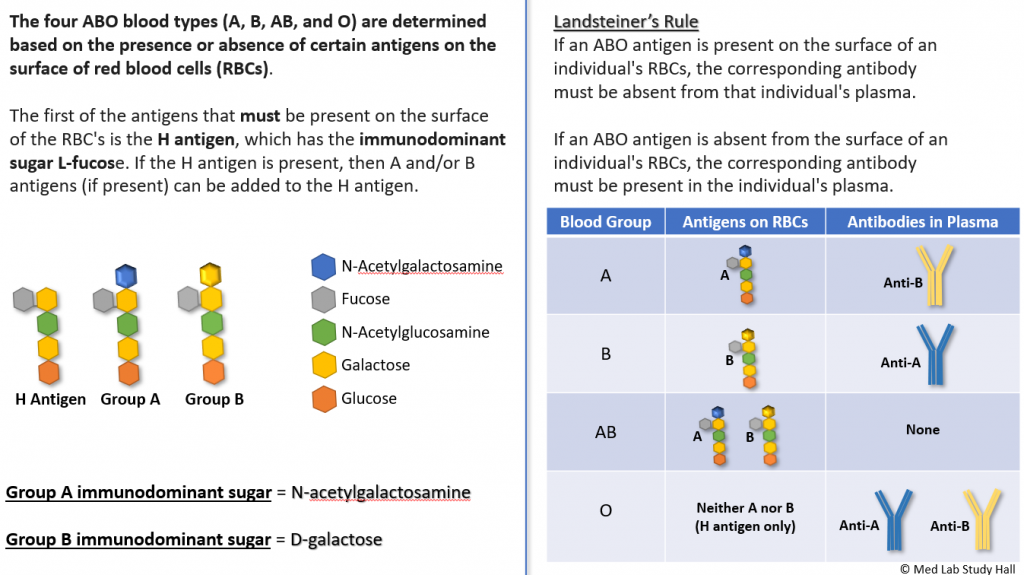
NOTE – It is possible for the H antigen to be absent on the surface of someone’s RBCs. However, this is an extremely rare occurrence and will not be discussed in this blog.
So how do we determine what blood type someone has in the medical laboratory? We do this by performing both a forward and reverse typing in the Blood Bank. Forward typing determines the presence or absence of A and B antigens on RBCs, while reverse typing demonstrates the presence or absence of anti-A and anti-B in plasma.
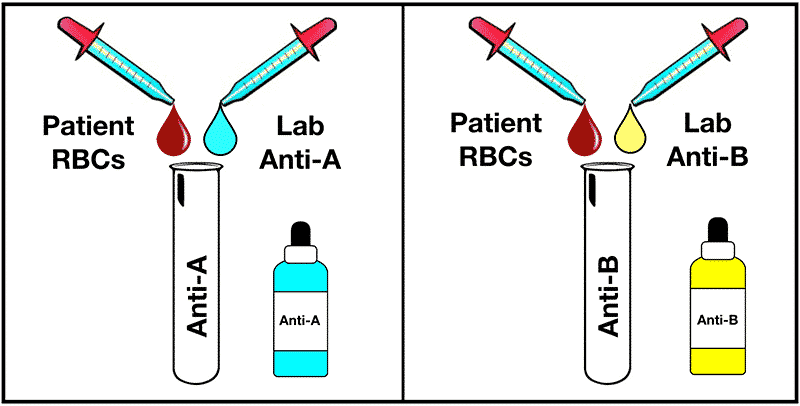
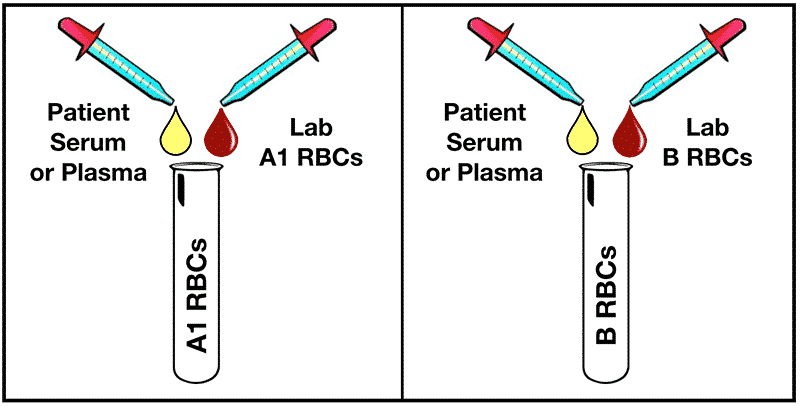
Most of the time, the forward and reverse typings agree with each other. As an example, if the forward typing shows a patient is ABO blood group A (agglutination with Anti-A, but no agglutination with Anti-B), the reverse typing also shows blood group A (no agglutination with A1 cells, but agglutination with B cells). However, this is not always the case. Hence, the purpose of this blog.
Let’s see what causes these ABO discrepancies.
Type A subgroup
Not all type As are created equal. Roughly 80% of patients with type A blood are A1, but 20% are a subgroup of A, mostly A2. There are both quantitative and qualitative differences between them. The A1 enzyme is much more effective at adding the immunodominant sugar to the precursor substance on red cells. This means there are many more antigen sites on A1 red cells and more H substance on red cells of the A subgroups. The red cells of A2 patients will react with anti-A, but may have a weak reaction, or may not react at all. The structure also differs and the patient can create anti-A1, which will react with the A1 reagent cells.
Suspect a subgroup of A when the forward type is A, but there is anti-A1 present. Less common, if the forward type is O, but there is no anti-A1 present.
When a subgroup of A is suspected, the red cells should be tested with A1 lectin (Dolichos biflorus). Lectins are plant substances that bind carbohydrates and A1 lectin binds specifically with A1 red cells. If the test is negative, that means the patient is a subgroup of A.
If the patient has developed anti-A1, red cells for transfusion can be chosen by compatibility at the AHG phase. Anti-A1 is generally a naturally occurring IgM antibody that reacts at room temperature and 37C. Transfusion reactions are not likely.
Cold reacting antibodies
If the patient has a cold reacting antibody, such as anti-M, or a nonspecific cold antibody, this can cause a false reaction in the reverse type. The reagent cells may be positive for the corresponding antigen and, therefore, react at room temperature. If the antibody is strong enough, the patient’s cells may even be agglutinated when you receive the sample.
If a cold reacting antibody is suspected, the patient’s red cells can be washed with warm saline. If there are extra unexpected reactions with reagent cells, you may have to warm the patient plasma and reagent cells to 37C before testing. You can also try a different lot of cells, or change methodologies.
Weakly reacting or absent antibody reactions
Antibody production can be decreased in elderly or immunocompromised patients. This is one instance where a patient history check can be useful. ABO antibodies are usually IgM and react at room temperature or 4°C. The reactions can be enhanced by adding an extra drop or two of plasma and incubating the tubes at room temperature for 5-15 minutes. You can also try incubating at 4°C, but keep in mind that most people have low titers of cold antibodies, and may have false reactions.
Acquired B
This is usually seen in patients with some sort of digestive tract issue such as colon cancer or infection. It is only seen in patients who are type A. Enzymes from intestinal bacteria modify the sugar on the red cells. The immunodominant sugar on type A cells is N-acetyl-D-galactosamine, and it is modified to become D-galactosamine. Anti-B detects the immunodominant sugar on B cells, which is D-galactose. The two sugars are close enough structurally that the D-galactosamine reacts with anti-B.
The patient will forward type with a weak anti-B reaction, but the reverse type will have anti-B. The patient’s red cells will NOT react with the anti-B in their serum. The condition will resolve with the resolution of the disease.
Transfusion related discrepancies
When a patient receives non-type specific red cells, you will often see a mixed field reaction caused by the separate populations of circulating red cells. If large volumes of plasma are given, reaction strength may weaken, or there may be extra reactions, depending on the amount of anti-A or -B in the donor plasma.
Investigation
Investigation of a discrepancy should always involve verification of your specimen, reagents and patient history. Never assume that the most obvious answer is the correct one.
- Verify the identity of the specimen and labelling of tubes, gel cards, or wells.
- Check the patient history for strength of previous reactions, recent transfusions, antibody history, diagnosis, and pregnancy. Ask these questions: Is the patient elderly, or had weak reactions before? Has the patient received non-type specific transfusions? Have they been treated at another facility where you can obtain history?
- Confirm that your reagents are in date and at room temperature before use. Check the labels-did vials get put back in the wrong place? Check reagent cells for hemolysis or small clumps that can be a sign of contamination.
- Review for technical errors: did you add all the reagents? Is it possible that tubes were reversed? Is your cell suspension too light or too heavy? Did you use the proper volume?
- Confirm proper function of your centrifuge.
- Always repeat the test to see if the discrepancy is reproducible.
- When deciding which reactions are the true reactions, generally the strongest reactions are correct. So if the A1 cell is weakly reacting, but the anti-A is 4+, then consider an A subgroup.
In Summary
It doesn’t take long before you will be able to spot a discrepancy a mile away. Resolving the discrepancy may take a little time or some trial and error. Think it through, consider the likely causes, and take a systematic approach.

